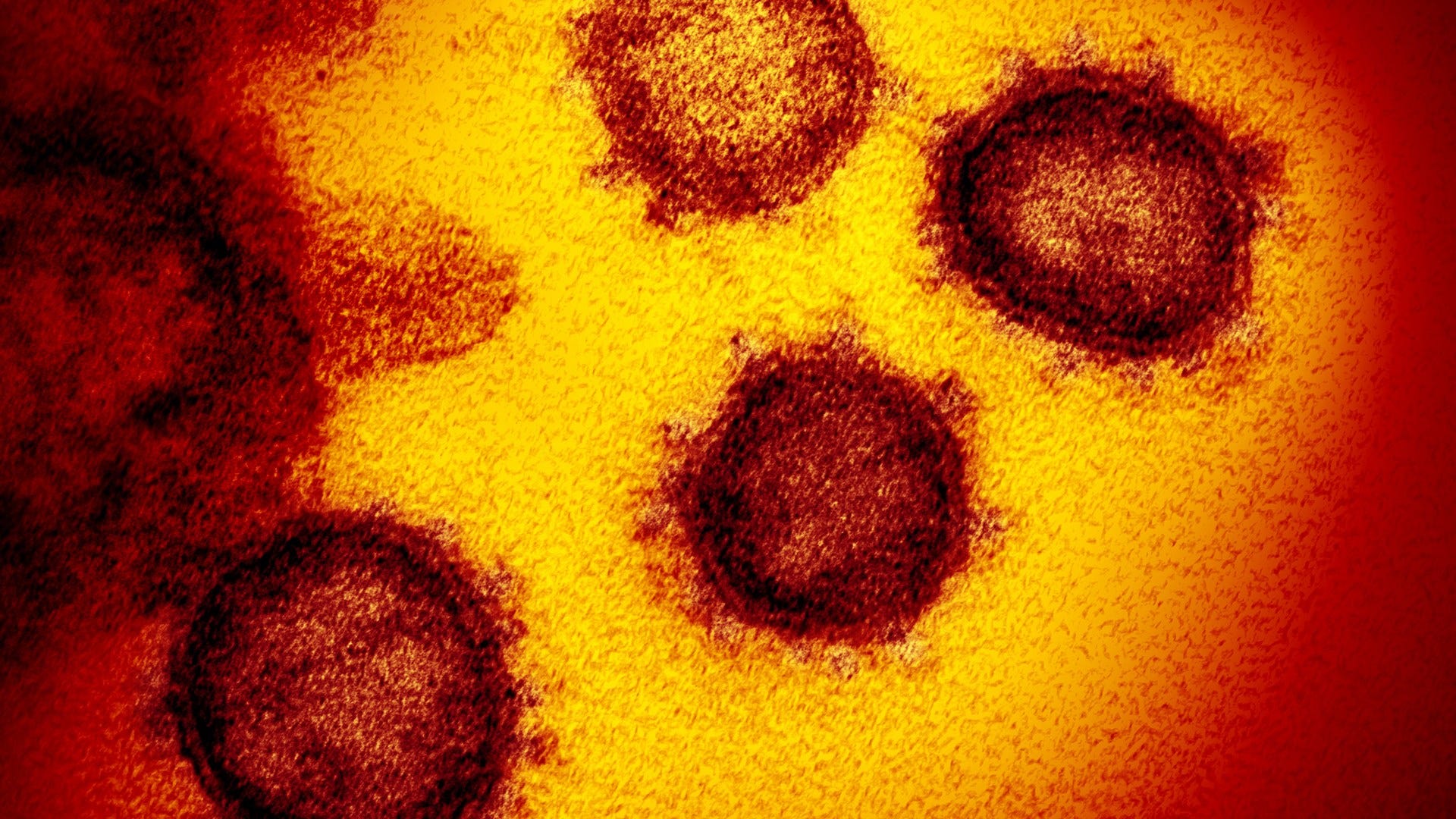
The immune formula of some other people who have not been exposed to the new coronavirus may be familiar with the pathogen, which will help decrease the severity of the disease if that user contracted COVID-19, suggests a new study.
The study, published in the journal Nature on Wednesday, found that of a pattern of 68 healthy adults in Germany who had been exposed to coronavirus, 35% had T cells in their blood that were reactive to the virus.
T cells are a component of the immune formula and help the framework of infection. The reactivity of T cells suggests that the immune formula would possibly have reveled in fighting a similar infection and would possibly use this reminiscence to help fight a new infection.
So how is it possible that your immune formula has reactive T cells if you had never had COVID-19? They were “probably acquired in past infections with endemic coronavirus,” researchers wrote, from establishments in Germany and the United Kingdom, in the new study. The use of this reminiscent of T cells from some other similar infection to respond to a new infection is called “cross-reactivity”.
“The big question is Array … perceives the role of these T. Array cells The study found that coronavirus reactive T cells were detected in 83% of patients with COVID-19.”
Although researchers also discovered pre-existing cross-reactivity T cells in healthy donors, they wrote in the study that the effect these cells can have on the final results of COVID-19 disease is still unknown.
The effects of the examination actually require more research, said Dr. Amesh Adalja, principal investigator at johns hopkins University’s Center for Health Safety, who was not interested in the retest.
“In this study, there appears to be a significant proportion of Americans who have this cross-reaction T-mobile immunity as opposed to other coronavirus infections that could possibly have an effect on how they deal with the new coronavirus. I think the big consultation is to check to jump from the fact that they have those mobile Ts to perceive what the role of those mobile Ts might be,” Adalja said.
“We know, for example, that young people and young adults are relatively unaffected by the serious consequences of this disease, and I think a speculation might be that the pre-existing T cells that exist would possibly be much more or more active at a higher level. older cohorts than in older cohorts, ” said Adalja.
‘What if you could also compare others who might have serious and benign illnesses and take a look at those other people’s T cells and say, ‘Are there other people with a serious illness who are less likely to have a cross-reaction? cells that other people with mild disease? more cross-reactivity T cells? I think there’s a biological plausibility for this hypothesis, ” he said. However, it is clear that the presence of T cells does not prevent other people from becoming infected, but does it modulate the severity of the infection? That turns out to be the case.”
So far, the coronavirus pandemic, the concentrate has been on COVID-19 antibodies and the role they play in strengthening immunity to the disease.
But infectious disease expert Dr. William Schaffner, a professor of preventive medicine and infectious diseases at Vanderbilt University School of Medicine in Nashville, who is not concerned in the new study, said T cells cannot be overlooked.
“Here’s an exam suggesting that there might possibly be some cross-reactivity – some pump priming if you will – with general traditional coronaviruses that cause colds in humans and possibly there would be some cross-reactivity with the COVID virus which is the cause It’s intriguing in itself because we had the idea, from the point of view of antibodies , that there weren’t many crosses at all, Schaffner said.
“It’s not entirely unexpected because everyone is members of the same family. It’s like they’re cousins from the same family,” he said. “Now we want to see if this has an effect on clinical practice. Array … does this make it more or less likely that the inflamed user with COVID actually expands a disease? And does this have implications for vaccine expansion? “
“Almost everyone else in the world had an encounter with a coronavirus,” added Adalja who was not surprised to see this cross-reactivity of T cells by examining participants who had not been exposed to the new coronavirus, called SARS-CoV- 2Array
“SARS-CoV-2 is the seventh human coronavirus to be discovered, and 4 of human coronaviruses are what we call community-acquired coronaviruses, and in combination those 4 are to blame for 25% of our colds,” Adalja said. “Almost every single user in the world has had an encounter with a coronavirus, and since they are all components of the same family, some cross-reaction immunity develops.”
Nature’s new study is not the only article that recommends a pre-existing immunity safe in others who oppose the new coronavirus.
Alessandro Sette and Shane Crotty, both from the University of California, San Diego, wrote in an article published in the journal Nature before this month, that “20 to 50% of unexposed donors exhibit significant reactivity to SARS-CoV-2 “antigen” peptide groups, based on separate research, however, noted that the clinical relevance of the reactivity remains unknown.
Sette and Crotty wrote that “it has now been established that the pre-existing immune reactivity of SARS-CoV-2 exists to some extent in the general population. It is assumed, although proven, that this may simply be due to the immunity opposed to “The non-unusual cold”. Coronavirus.
The-CNN-Wire ™ and © 2020 Cable News Network, Inc., a WarnerMedia company. All rights are reserved.