Sheria Robinson-Lane, assistant professor and gerontologist specializing in palliative care, long-term care and nursing management at the School of Nursing; Samuel Bagenstos, law professor Frank G. Millard; and Jason Pogue, a clinical professor of pharmacy, talks about mandatory vaccines and vaccine safety.
Can employers legally require health care to provide evidence of safe vaccines as a condition of employment?
Robinson-Lane: Yes, you can. Vaccination is most likely a federal regulatory requirement for establishments that earn Medicare and Medicaid investments. Lately they require weekly staff tests.
As a general rule, anyone who has direct contact with patients will be vaccinated, adding nurses, practical nurses and activity staff. Homework staff enter and leave the rooms, so they would also be included in these measures.
Currently, an annual flu vaccine is required. Some amenities will allow workers to opt out of receiving the vaccine and wear a mask during flu season, regularly from October to March. These workers can’t do much if they don’t have a medical challenge that makes it irrelevant. If you need to work, you get vaccinated. Adults in institutional care are highly vulnerable to respiratory infections such as colds, flu and coronavirus, so these measures are mandatory to ensure their safety.
Robinson-Lane: I don’t know all the must-have staff. This might be highly recommended, but I don’t see the local merchant or Internet service provider applying the COVID-19 vaccine to their employees. However, I think it is realistic that physical care staff see a long-term vaccination mandate if they provide direct care.
Bagenstos: Maybe. Under the Americans with Disabilities Act, an employer may require a vaccination only when doing so is “job-related and consistent with business necessity.” Whether an employer may require a vaccination thus will turn on such questions as: (a) whether state governments require workers to be vaccinated, (b) whether the employee works in a particularly high-risk setting and (c) the effectiveness of the vaccine. And an employer will be required to provide reasonable accommodations to workers who have medical conditions that make them unable to take the vaccine. Those accommodations might include reassignment to a job where there is less risk of transmission of the virus.
Robinson-Lane: Many of the must-have employees who serve seniors in nursing homes and rehabilitation services identify as black, aboriginal, or other people of color. There is still a bit of medical and pharmaceutical mistrust among these communities, and there is widespread fear that these vaccines are not or are not tested very well before they are forced to take them. Workers don’t need to be anyone’s guinea pig. I think what has increased fears among these teams is the initial reaction to the virus that has left many establishments suffering to locate enough PPE for staff and expand staggered infection policies, as well as converting regulatory rules that take into account access to supplies. , like N95 masks, not just safety.
What steps is the FDA taking to make sure a vaccine is for the public?
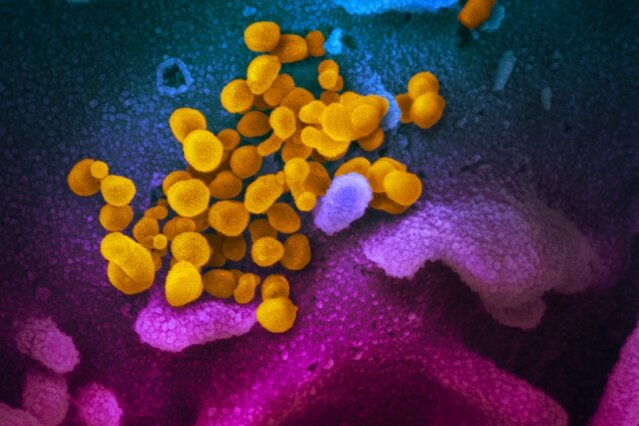
Pogue: The procedure for making any vaccine is performed in 3 stages of human testing. Phase 1 is largely a dosing and protection study. It is performed in a small number of healthy patients to ensure that there is an immune reaction (we are appearing antibodies) and that there is no apparent protection problem. Phase 2 accelerates this in a larger population. Phase 3 is the one we recently entered. These are much larger studies with the dosage regimen that has been subtle in past stages. Because of the length of this study, we can make sure more of the vaccine protection, as well as perceive how much it works to save the disease (it is one thing to expand the antibodies, and another is to see if the production of those antibodies leads to the salvation of diseases).
In addition to better understanding the frequency of non-unusual adverse occasions (fever, injection site pain, “flu-like symptoms”), by recruiting so many patients in these studies, we can identify if there are any, still serious and affected adverse occasions. This protection data is then combined with knowledge about the effectiveness of the vaccine in preventing disease and is used through the FDA to approve or not the use of the vaccine. So, whether the vaccine comes from the U.S. Or from abroad, those same types of Phase 3 knowledge (and Phases 1 and 2) will be used to make the decision.
How is safety enforced in the states if the vaccine is developed overseas?