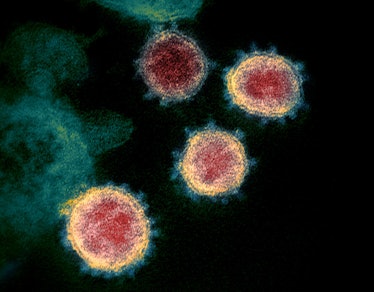
You can get coronavirus twice — scientists explain why.
On Monday, scientists reported the case of a Nevada man dealing with a frustrating new progression in the story of Covid-19. The 25-year-old appears to have the coronavirus a moment after recovering. This is the first demonstrated case of “reinfection” reported so far in the United States.
According to the report, the patient first experienced symptoms such as sore throat, cough, fever and headache in March, and was tested for Covid-19 in April. By the end of April, his symptoms had disappeared, and as of May he had tested negative for coronavirus, twice.
However, on May 28, the patient started to feel sick again, this time reporting headaches, fever, cough, dizziness, diarrhea, and nausea. By June 5, he tested positive and showed signs of hypoxia – a low level of oxygen in the blood. The patient was then hospitalized, where he continued to receive oxygen. These findings were published in the journal The Lancet Infectious Diseases.
This is the first case of coronavirus reinfection. To date, at least 4 cases of reinfection have been demonstrated, adding that of the patient from Nevada: a case of asymptomatic reinfection in Hong Kong, a case in Belgium where the patient had milder symptoms, and a case in Ecuador, where the patient felt worse at the time he was infected with Covid-19.
These show that Covid-19 infections cannot provide each and every user with surely foolproof coverage against a new disease. This isn’t unusual, says Stephen Goldstein, a postdoctoral researcher and evolutionary virologist at Utah University Health. He was not involved in the study.
“We already know that no infection produces 100 percent protective immunity in 100 percent of people. This is even more demonstrated in the case of respiratory infections,” Goldstein explains to Inverse.
This article, he claims, also demonstrates that herd immunity without a vaccine is an option. This is one of the many clinical and moral reasons why herd immunity is practical.
However, we don’t rely only on natural immunity against the virus: hopefully, we will soon have a vaccine that will be the immune formula against Covid-19 and will finally help end the pandemic.
This article does not derail that quest; This underlines how vital this is.
A timeline of this patient’s coronavirus symptoms.
Developing symptoms twice is not enough to lead to reinfection. It was genetic research that made it possible to verify this case. The study reports that the patient was infected with another variant of the virus at the time.
It’s vital to note that the lifestyles of this variant alone don’t mean we want more than one type of vaccine to fight the coronavirus, as Yale immunologist Aikiko Iwasaki noted in an accompanying commentary. Studies on the genetics of existing SARS-CoV Two variants suggest that their genetic diversity is quite low, implying that those circulating recently should not exceed the performance of a single vaccine. Iwasaki writes:
“There is currently no evidence that a SARS-CoV-2 variant has emerged as a result of immune evasion [evolving to get around the immune system]. For now, one vaccine will be sufficient to confer protection against all circulating variants.”
The paper’s lead author, Mark Pandori, director of the Nevada State Public Health Laboratory, shares Iwasaki’s assessment. However, he also warns that it is still difficult to establish the connection between the genetic adjustments of the virus and how our immune formula fights it.
“While genetics is a useful way to detect reinfection, it’s incredibly tricky to know if it translates into structural changes that would have an effect on immunity,” he told Inverse.
Goldstein suggests that we take a closer look at the immune system, not the virus itself. We don’t actually know how this person’s immune system reacted to the coronavirus the first time – a major limitation of this study.
The one about coronavirus.
“A small percentage of people will fail to mount a good immune response to any infection,” says Goldstein. “With tens to hundreds of millions of SARS-CoV-2 infections there will be a lot of these people even at a low rate, and these people probably are more susceptible to second infections.”
It suggests that reinfection within 40 to 60 days of the first infection would likely imply that a strong immune reaction did not spread on the first attempt. The Nevada patient tested positive twice in 48 days.
“But at the moment this is a hypothesis,” he warns.
That’s why a vaccine is so important: it aims to get the recipient to develop a strong immune reaction the first time.
Pandori emphasizes that we can’t use this article to wait for how a vaccine might boost the immune system.
“Vaccine-based immunity is different: it can be higher and develop over time,” Pandori says. “So we’re waiting to see that. “
The likelihood of reinfection: Goldstein suggests that the vast majority of people will likely develop a strong immune reaction the first time they encounter the coronavirus.
“The fact is that the vast majority of COVID-19 patients probably have strong protective immunity for up to 6 months and some coverage thereafter,” he says.
That said, those cases highlight that strong, protective immunity is not the case. Until there is a vaccine that proves it allows the immune formula to respond to the virus, other people will have to wear masks, with or without antibodies.
This article was originally published on October 13, 2020.