As experts in pandemic policymakers, we sense the strain that coVID-19 and influenza mixture can have on our health care system. Our new report, COVID-19 and Seasonal Influenza: Preparing for a Collision, newly published through the Scowcroft Institute of International Affairs at Texas A-M University, explains the dangers and makes 10 recommendations.
Figures one autumn and winter dicy
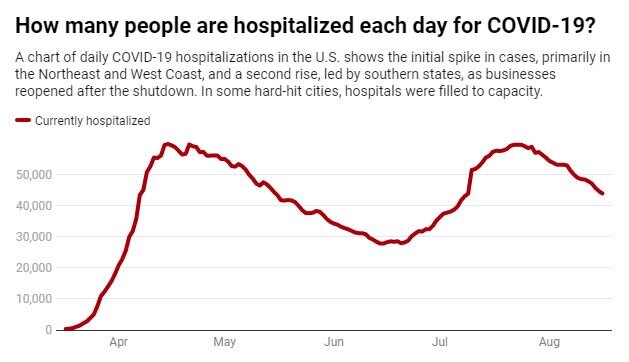
Nearly five million more people in the United States have become inflamed with SARS-CoV-2 and more than 170,000 have died. In some hospitals, such as the Starr County Memorial on the Texas-Mexico border, the number of cases exceeded capacity.
Because COVID-19 and influenza breathe viruses that require similar materials and equipment, hospitals that are already suffering to accommodate COVID-19 patients may not be able to handle more influenza patients.
Influenza-related hospitalizations have ranged from a minimum of approximately 280,000 in 2015-16 to a peak of 810,000 in 2017-18. According to the knowledge of the American Hospital Association, as of March 2020, the United States had a total of 924,107 hospital beds. If a city or state has become a focus of flu and a focus of COVID-19, it would almost overwhelm the hospital’s capacity.
In addition, some of the measures that have been effective in managing the maximum capacity of the hospital, such as the use of Texas Children’s Hospital in Houston for adult patients with COVID-19, would possibly not be conceivable as young people under five are one of the teams.maximum maximum likely to have severe seasonal influenza results, adding hospitalizations and deaths.
Like the threat of a double blow.
Faced with the threat of a bad season to COVID-19 and the influenza that is overwhelming the capacity of US hospitals, it is not a threat to the us.Our report makes 10 recommendations.