Maxanne McCormick had any and all explanations for why she was dying of the same degenerative dementia that killed her mother. She was diagnosed in 2011, when she was in her fifties: a devastating explanation for more than a decade of migraines, pain, and mental confusion. And the fatigue was so overwhelming that he had to abandon his task as a medical assistant. Once, at the beginning of his illness, he had just arrived at work at a pediatric work center in Littleton, Colorado, and was struggling to hang up his plaque. – a stupid and crazy task he had done a million times – when his arm froze, then he started struggling.
After his diagnosis, he enrolled in a study at the University of California, San Francisco that accumulated some of the most comprehensive knowledge ever compiled about his condition. Its biannual westward walks have allowed clinical researchers to measure its decline. With each trip, his physical condition deteriorated. He lost the ability to walk and then talk. Eventually, needing 24-hour care, Maxanne left the home she shared with her husband for a nursing home, where she is the youngest resident in decades. “Essentially, I’m waiting to die,” he recalls. He read a book called Final Exit to help weigh the merits of physician-assisted suicide.
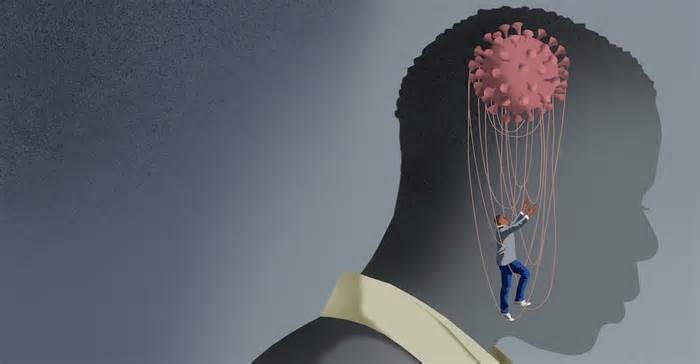
In early 2016, he took another vacation at UCSF. It started like any other, with assistants escorting Maxanne in wheelchairs through the Denver airport and to the study hospital, where students ran days of testing as they have. do. But this time, when they gathered the team for a report, they shared an unforeseen discovery: They no longer believed he had degenerative dementia. His MRIs seemed too solid for that. Instead, he suffered from something called Functional Neurological Disorder, or FND: a brain processing challenge that can lead to significant pain throughout the body without damaging corresponding tissues. So-called functional symptoms are strongly correlated with psychosocial misery and can be unbearable, despite avoiding maximum laboratory testing. Conceding that we lack the vocabulary to perceive how the brain interacts with the rest of the framework, most FND scholars use the metaphor: FND is a software challenge, not a hardware challenge. It’s not the device itself that’s broken, but the formula that makes it work.
Maxanne told me all about FND early one morning on Zoom, her brown mane almost washed out in the sunlight streaming through her home workplace window. After years of suffering to come to terms with her faulty hardware, she said, she was determined to do whatever it took to reset her software. He launched himself into retraining exercises that he was cautiously told might help retrain his brain: he took aim at his symbol reflected in the mirror, seeking to direct the symbol to fulfill responsibilities he had long failed to force upon his own limbs. To do it. . Maxanne’s tone (she’s “Max” to her friends, blog readers, and news lovers) gradually shifted from planned and clinical to fast-paced as she told this component of the story. “The initial healing was nothing short of miraculous,” she told me. Her speech returned immediately. Within a week, she was walking again, first around the house, then around the block, then down the aisle to her youngest daughter’s wedding. “Of course it was difficult being around a lot of people and noise and things like that,” she said. Even today, things are not perfect. Her tremors are accentuated when she is stressed, for example, and she sets appointments in the morning to anticipate tiredness in the afternoon. She demonstrated how her frame still plays tricks on her: she may have just gently touched her nose when she pointed at my face on her screen, but she winced when she paid attention to her own arm.
However, Maxanne may not have been the last time she felt so good, when she had recently been so sure she would never feel well again. She read all she could about the NDF, dismayed to have heard so little about it. even as a fitness professional. And he had an overwhelming need to share what he had learned with everyone languishing with symptoms similar to his own. He began writing a blog about his recovery and temporarily became one of the most prominent people in the world. public living with the NDF. ” It’s become kind of a project of my life,” he told me. “I care so much about helping other people who are stuck on this damn path. “
But not everyone is satisfied with her work, adding to many other people Maxanne Maximus hoped to achieve, whose ailments are eerily similar to hers. or ME/CFS; chronic Lyme disease; and, more recently, long ago Covid: they fiercely reject NDF as tantamount to telling patients that all their suffering is in their heads. Jennifer Brea, ME/CFS activist and documentary filmmaker, insists that FND is “not a primetime diagnosis. “. Other proponents say it’s an acronym for “fictitious non-diagnosis. “They say their ailments are strictly physical; the concept that your intellectual fitness possibly has something to do with your symptoms is as offensive as viewing HIV as anxiety.
These debates have been supercharged by the rise of the long Covid, a term coined through patients evoking a chronic postviral illness that persists after those affected have apparently recovered from SARS-CoV-2. New Covid activists have long been associated with ME/CFS champions and similar diagnoses, studies on biopharmaceutical interventions are no easier than psychosocial studies and support. The clash shows strong tensions between biomedical and biopsychosocial models of medicine that address basic questions about what disease is and what medicine it can and cannot do.
Symptoms like Maxanne’s (excessive fatigue, pain, involuntary tremors and spasms, dizziness, mental confusion and malaise) have persisted in history and medicine has never really known what to do with them.
Since the disease is largely socially defined, understanding of express diagnoses has been fluid in time and space. But the ultimate direct precursor to NDF is anything you’ve probably heard of: hysteria. For most people, “hysteria” evokes an obnoxious ancient relic: Hippocrates’ edition of “Women Are Mad. “But while the diagnosis of hysteria undeniably has misogynistic roots, the ancient Greeks were convinced that uteruses migrated from the frame and caused all sorts of symptoms, and doctors retained the hysterical Greek root as their “womb” when they conceived of an amalgamated disease centuries later: hysteria as a coherent medical category was also thought of as a real, depressing disease that devastated women in various ways. disproportionate, but it also affected men.
At the end of the nineteenth century, Jean-Martin Charcot, the so-called father of neurology, became intensely interested in hysteria. While the cases shared non-unusual symptoms with other situations he had described, such as sclerosis and Parkinson’s disease, the latter patients had telltale brain damage that necessarily matched their symptoms, unlike hysterical ones.
But soon, paintings about a Charcot student’s hysteria overshadowed his own. Sigmund Freud concluded that the long-observed correlation between trauma and hysteria was a direct causal link to an equally undeniable solution. Simply put, hysteria was subconscious conversion. from repressed painful memories, occasionally sexual in nature, into physical symptoms, and patients can simply their illnesses, Freud insisted, through recall and psychoanalysis. (When those strategies failed, Freud had all sorts of complicated explanations. )
Freud’s influence helped divide neurology and psychology into separate camps, condemning hysteria to discomfort between them. And in 1964, the diagnosis gained a primary public blow that diverted clinical interest. A British psychiatrist, Eliot Slater, reviewed the medical records of dozens of patients with hysteria. who had passed through his hospital and found selected diagnoses for each. At a now-famous medical conference, he absolutely criticized the structure: “The only thing that can be shown that hysterical patients are not unusual is that they are all patients. . . . The diagnosis of “hysteria” is a disguise of ignorance and a fertile source of clinical error. In fact, this is not just a ghost but a trap.
Slater’s ancient findings are still hailed by those who are convinced that hysteria was nothing more than a dismissive label applied to physically ill women. , reports began to emerge of patients being left with persistent symptoms long after a Russian flu epidemic in 1889. A similar trend followed the Spanish flu of 1918. she appeared dozens of times, adding at a Wisconsin convent, at an Athens midwifery institute and among nurses at a London hospital. In 1984, in the thriving ski town of Incline Village, Nevada, on Lake Tahoe, more than in the past, healthy patients suffered from generalized tiredness. Stung a compelling single cause.
It’s the well-known Lake Tahoe cluster that the Centers for Disease Control and Prevention first named chronic fatigue syndrome, now more commonly known as ME/CFS (which is a compromise between the original call and “myalgic encephalomyelitis. ” , a term favored by patients who argue that “chronic fatigue” does not reflect the severity of their condition). In the face of decades of stigma, comedian Ricky Gervais mocked ME/CFS in 2007 as “the one where ‘I don’t feel like going to paint today,'” advocates and a core organization of committed researchers have Yet they forged a framework of wisdom about a disease they say gets the least laugh, relative to its burden, from the National Institutes of Health. A survey showed that more than 70% of patients surveyed said an infection triggered their illness, and the diagnosis includes symptoms such as excessive fatigue, sleep problems and pain. Its diagnostic determination criterion is post-exercise malaise, that is, a significant loss of power after a physical or intellectual effort. For the past several years, the CDC website has included a disclaimer in its ME/CFS policy: “ME/CFS is a biological disease, not an intellectual disorder. ME/CFS patients do not simulate or they look for secondary gains. These patients provide multiple pathophysiological settings than multiple systems. “
The CDC was destined to the max to scold other people like Michael Sharpe. In the 1980s, when the Emeritus Professor of Psychological Medicine at Oxford was still a junior researcher, a fellow infectious disease specialist was mystified by patients suffering from unexplained exhaustion and pain. Sharpe spent months at this clinic, gathering and listening to patients, taking detailed histories, and reviewing the popular lab tests they had received. And while he may not say for sure why they were still so sick, he noted that those in the most pain tended to focus intently on their symptoms, worried they weren’t getting better and very worried they weren’t going. to get older. anything to ease their ailments. worse. Some were so distraught that he beat them. They have even moved away from things they once enjoyed. “That’s how they gave me to wrap,” he told me. “I always wanted to see if we could do things for these patients that medicine can’t. You know, is there a way to come from some other angle here? In that case, any other behavioral angles besides doing a lot of blood work? When cognitive behavioral treatment seemed to help other people with other conditions, Sharpe wondered if he, too, could help patients whose symptoms, however severe, were not compatible with pathophysiological rules. In one essay, he called it “disease without disease. “
It turned out there were many such patients, and Sharpe passed on his fondness for treating them to his young neurologists, Jon Stone and Alan Carson. By the 1990s and early 2000s, it was clear that past illnesses known as hysteria had disappeared. not only did it disappear, but it was classified into more suitable diagnostic categories, as Eliot Slater had called it decades earlier. Stone and Carson began reading the symptoms through a neurological lens, conceiving them as failed brain signals rather than a Freudian cry for help. To change the name of hysteria to FND was to reject the concept that the most productive way to perceive service as anal paralysis was as a subconscious suppression of memories of formative years. Rather, it was an interruption in brain processing that facilitates executive service of the legs, an abnormality that can be activated through all sorts of things.
In other words, tension may simply exacerbate NDF, and a user with NDF may simply focus on the symptoms and necessarily increase their volume, requiring brain processing for movements that deserve to be automatic. As Carson told me, the term “functional neurological disorder” deserves to be reserved for neurological symptoms such as weakness, seizures, memory loss, or cognitive problems. Functional symptoms” and “functional disorders” are used interchangeably for other parts of the body. Irritable bowel syndrome, for example, is widely theorized as a functional disorder. Meanwhile, situations like depression and anxiety occasionally come with symptoms that most people would describe as physical. It is even imaginable to have functional and non-functional symptoms at the same time. “We wonder why other people are confused!” Carson joked.
While defining those concepts can be tricky for the experts who spend most of their time on them, create what is beyond other doctors. About 20 years ago, Dr. Mark Hallett was stunned by how poorly medicine treated such cases. As a lead investigator at the NIH’s National Institute of Neurological Disorders and Stroke, he invited referrals from physicians across the country over decades of difficult-to-diagnose patients presumed to have rare neurological diseases. “I started to feel like we were seeing a lot of what we call ‘psychogenic’ at the time,” Hallett told me. “About 30% of our cases had a functional diagnosis. And I said, ‘Damn, this is a primary problem. ‘” In 2006, Hallett went on to describe the inability to capture those non-usual manifestations of disease as crisis medicine.
“I started looking into the existing landscape, and it turned out there was very little about functional disorders,” he told me. “Very few textbooks, very little teaching. There were virtually no studies underway. No one had much interest.
In 2020, that’s for good.
In the early days of the Covid-19 pandemic, the contours of a now-familiar story began to unfold. After getting swollen with the new coronavirus, some other people have not recovered as temporarily as expected. In mid-April 2020, journalist Fiona Lowenstein published an op-ed in The New York Times titled “WE NEED TO TALK ABOUT WHAT CORONAVIRUS RECOVERIES LOOK LIKE”. Lowenstein had founded a survivor support organization for others whose symptoms still had not cleared up after several weeks. Soon, an infectious disease specialist at the Liverpool School of Tropical Medicine, Paul Garner, wrote a series of blog posts for the British Medical Journal about the harrowing consequences of his Covid-19 illness: “For 7 weeks I went to a roller coaster. of poor health, excessive feelings and total exhaustion,” read one headline. In subsequent articles, he described intense brain fog, tinnitus, and a bad relapse after taking an aerobics class: “I was more exhausted than ever and couldn’t get up for 3 days,” he wrote, an accurate description of “post-morbid malaise. ” effort”. ”, I did not know at the time. In June 2020, Lowenstein and Garner were key resources for Pulitzer Prize winner Ed Yong’s first Atlantic article on what patients on online help teams soon called “long covid. “
Other stories of Yong and many others followed, and the picture they painted was terrifying. People who had relatively mild initial episodes of Covid-19 were in very poor condition weeks, months, and even a year or more later. One of the first features described other people suffer from “immoderate fatigue, bulging veins, excessive bruising, abnormal heartbeat, short-term memory loss, gynecological problems, sensitivity to light and sound, and brain fog. “Others have developed new allergies and immoderate itching, episodes of blindness and paralysis, or joint pain and hair loss. Many patients became ill after asymptomatic cases of covid-19. After other people who were slow to recover began collecting online, a survey found two hundred symptoms related to the emerging disease.
Almost immediately, ME/CFS advocates identified what was happening: they thought Long Covid was just the newest wave of their own disease, which followed a viral infection. Thanks to the scale of the coronavirus pandemic, their lifestyle was more undeniable than ever. As Jaime Seltzer of the advocacy organization MEAction told WebMD, if the proportion of other people ending up with a long-term illness is “similar to what has been observed for other pathogens, then we foresee a massive disability event. “Subsequent studies advised that some other people with persistent symptoms after Covid-19 met the diagnostic criteria for ME/CFS. Seeing common cause, existing advocacy networks have long allied with new Covid advocates. MEAction has reportedly contacted many bloodhounds and doctors. since the beginning of the pandemic to highlight the link between ME/CFS and the long Covid.
Almost 3 years after the SARS-CoV-2 pandemic, their arguments have the consensus of experts around the world, shaping the public and professional understanding of the long Covid as a complex, chronic and biological disease overlooked through science. Meanwhile, so much studies have accumulated suggesting a physiological disorder similar to prolonged covid that some other people have begun to wonder if the total number of prolonged covid exceeds that of an acute illness. Oxygen brain, and even the Epstein-Barr virus, which there is strong evidence that causes multiple sclerosis.
More recently, a study by Yale immunologist Akiko Iaki and Mount Sinai physiotherapist David Putrino provided more evidence of measurable physiological abnormalities in long-term Covid patients: reduced T cells, for example, and reduced cortisol levels. “We hope our study will be informative for others running in the field,” Iaki said on Twitter when the preview was released. “We also hope this information will help those who are still skeptical realize that prolonged COVID is real and biologically based. “
But Long Covid has never been as clear and dry as some quarterbacks have suggested. While advocates have noted recent years as too excessive a narrative of medicine’s perennial indifference to women and the diseases that disproportionately afflict them, others have noted anything else. : a dramatic depiction of the suffering caused by psychosocial distress and how ill-equipped medicine is to handle it.
This more recent case looks like this: a chronic illness that seemed to be triggered through a viral infection may also have been triggered just as easily through the trauma of the pandemic itself. It possibly stems from the fact that, in a patriarchal world, women face more adversity and have less over their lives.
The overwhelming variety of long-lasting problems from Covid raises the question of whether all of them are attributable to a viral infection, especially since two of the most reported symptoms, fatigue and brain fog, are also commonly linked to stress, depression, anxiety and pain. Asal problems. problems like FND. Since 2019, the rates of other people with depression and anxiety have quadrupled, by some estimates; loneliness and isolation have also increased. A recent study found that all of those things were strongly linked to long covid. Results at the cellular and hormonal level similar to those of the Putrino and Iwasaki test were also seen in chronic pain, post-traumatic stress disorder, and depression, but they do not appear to correlate with symptoms, and it is not clear what this all means clinically. or if there is a causal relationship. Finally, an NIH-sponsored longitudinal study of long-COVID, the most comprehensive and detailed study of the disease to date, found no damaged tissue in patients with long-COVID, no evidence of viral patience, and no organ abnormalities compared with the controls. “We found little to no abnormalities,” lead author Dr. Michael Sneller told NPR ahead of the study’s publication. “Echocardiogram, lung serve as tests, X-rays, brain MRIs. you call it Organ storage as laboratory markers. We see none of that. . . and little valuable evidence of immune activation. . . Basically, I’m running out of tests to do. However, one combination that his last article discovered was a combination between prolonged covid and anxiety disorder.
Moreover, the relationship between infection and long-term acute Covid illness seems tenuous. A first detailed cohort study conducted by the patients themselves found that although the availability of PCR tests was delayed at the beginning of the pandemic, most participants eventually underwent antibody screening. Tests: However, more than two-thirds of those participants tested negative, suggesting that even after accounting for false negatives and the option that antibodies will never materialize or disappear over time, at least some of them never had Covid-19 to begin with. Other long-term studies on Covid also raise questions: some widely cited studies did not use any control groups, made misplaced comparisons (e. g. , pitting long-term debilitated Covid patients against other healthy people rather than, say, other people with excessive depression), or were published in predatory journals that pay on edge with questionable peer review processes.
Meanwhile, there is evidence to suggest that some symptoms attributed to long-term covid may possibly be functional. Alan Carson, one of the leading neuropsychiatrists in functional symptoms, told me that he had noticed a lot of NDF and other functional disorders in Covid clinics for a long time in Edinburgh. Many studies lack detailed clinical trials by experienced clinicians, he told me, relying instead on brief sessions with admitting nurses and searches for new biomarkers. In one case, he re-examined long-term Covid patients who had undergone much shorter tests in an earlier study and uncovered context that other researchers had missed. He decided that a Covid patient who was unable to walk had functional paralysis that was likely triggered through his traumatic hospitalization at the start of the pandemic: “He had been awake and conscious for much of his time in extensive care,” he told me. carson. “And he’d been exposed to a lot of other people dying quite horribly, thinking, ‘Oh, I’m next. ‘ “For Carson, the concept that the etiology of this man’s symptoms would make him less worthy of attention or sympathy than someone whose symptoms are caused by physical tissue damage is troubling. Some other people are willing to ‘feel sorry’. by patients,” he said, only “if we locate a classical pathogenic mechanism. . . and that, to me, is fundamentally wrong. Period. “
Mark Hallett, the NIH physician, also observed functional symptoms in the long cohorts of covid and ME/CFS. “Some patients will have a biological etiology for their post-covid syndrome, other patients will have a functional etiology,” he tells me. Needless to say, each and every diagnosis is wrong. The functional disorder is not voluntary. People don’t do it themselves. It’s just the way the brain reacts to your specific situation.
The head, the only organ capable of experiencing any disease, and whose service as it is irrevocably affected by love, poverty, violence, refuge, despair. So, in that sense, maybe Covid is in your head for a long time. Like everything else.
Does this mean that long Covid is “all in your head”?In a sense, no, of course not. The symptoms are genuine and the testimony of patients about them is sacrosanct. They are not confused, rigged or unreliable. They are sick. But otherwise, the head constitutes the only organ capable of experiencing any disease – and whose service as it is irrevocably affected by love, poverty, anguish, violence, terror, geography, housing, monotony, despair, etc. There is no feeling or interpretation of anything outside your brain. So, yes, maybe Covid is in his head for a long time. Like everything else.
For all their disagreements, proponents of biomedical and biopsychosocial models of the long percentage of covid abound in unusual terrain. The COVID-19 pandemic has led to widespread weakness, either as a result of détente or the virus itself, aggravated in both cases by political neglect. and failures of public adequacy. Both sides stress that patients are suffering and that it is not their fault. Where they differ is in treatment problems.
By the mid-2000s, Michael Sharpe had spent years treating the kind of patients he first encountered at the Oxford Infectious Disease Clinic: other people with persistent chronic symptoms that undermined the brilliance of their lives. It may simply not make patients’ lives perfect. “This is essentially what we used to call rehabilitation,” he told me. “It’s about helping other people come to terms with the situation they’re in, giving them some long-term hope and helping them move forward gradually. “
In 2005, Sharpe began recruiting patients to participate in the largest clinical trial ever conducted of ME/CFS to see if his restorative strategies could also help those patients. The PACE trial examination protocol, which was designed in collaboration with a UK charity for ME/CFS patients set out to find out whether gradual training cure, or GET, and cognitive behavioural cure can improve outcomes. In 2011, Sharpe and co-authors published their response: GET and CBT in moderation improved fitness CFS patients. Few test participants achieved miraculous change, and some did not respond much, yet there was an undeniable if modest overall impulse. This made GET and CBT the only clinically validated remedy for ME/CFS.
Four years later, journalist David Tuller wrote a 15,000-word critique of the PACE essay, calling it “fake and terrible research. “Dozens of researchers, doctors and advocates have joined him. They wrote open letters to The Lancet calling for the retraction of PACE, discussed the factor at conferences, and condemned the trial in other media outlets. A lengthy legal war forced Sharpe and his co-investigators to hand over their data, which critics reanalyzed and claimed to have undermined PACE’s findings. Psychologist David Marks, editor-in-chief of the Journal of Health Psychology, summarized his objections to what PACE stood for: “Gaslighting has been implemented throughout the ME/CFS network through the application and misuse of the biopsychosocial model. “
Given PACE’s final mundane conclusion, the tenacity of the reaction is striking. “It’s pretty hard to think of a chronic illness where psychologically informed rehabilitation doesn’t help,” Sharpe told me. The same goes for a conscientiously graduated exercise. Today, despite the setback, Sharpe continues his investigation. “He was probably hammered like no other trial in history has been. It has been debated 3 times in the British Parliament. It’s still there, nobody killed it. Neither the Lancet nor the UK Medical Research Council has disavowed it. More importantly, he said, “some people’s lives will be broken because they may not have rehabilitation when they can, and that’s terrible. “
What he says is not an exaggeration. Proponents succeeded in getting GET and CBT removed from the official ME/CFS remedy rules in the U. S. They also opposed it as a remedy for prolonged Covid. now debunked” and warned that anyone who suffers post-exertion discomfort and strives to exercise can permanently worsen, a claim that is not based on evidence and would make the condition strangely exclusive in the annals of medical knowledge. MEAction is conducting a PSA crusade to distance the audience from PACE-validated remedies. Their online page includes links to anecdotes about patients who say they have had to lie down or use a wheelchair after short walks.
Worse still, peddlers and fringe charlatans would have started dispensing all sorts of unshown remedies and matching longtime Covid patients with questionable diagnoses requiring unsubstantiated tests and remedies. Some patients were prescribed blood thinners in case they cleared up “microclots” circulating in their bloodstream, and those drugs put them at unnecessary threat of serious bleeding. Shady proprietary corporations without peer-reviewed publications promise they can diagnose and treat the disease. Notorious ivermectin stalwarts turned to Covid for a long time. Furthermore, it is most likely that the exploitation of patients observed in ME/CFS and other contested diseases may soon be directed at a new population of people with chronic diseases. So-called Lyme literate doctors with invariably cash-based practices have misled patients with unnecessary testing and unsubstantiated interventions, such as long-term antibiotics that have continually proven useless and overused for disease-free patients. of Lyme shown. In recent years there has been a backlog of unapproved neurosurgery for ME/CFS, one of which is said to have left a young patient in the UK with disastrous complications.
For Maxanne McCormick, the former medical assistant who recovered from the worst of NDT with strategies similar to CBT and GET, the dicy remedies in which patients are absorbed are disturbing. But she understands how other people with health problems can feel abandoned through medicine: after all, she once felt that way, too.
When he began to fall ill, prior to his diagnosis of degenerative dementia, he was diagnosed with “conversion disorder,” the Freudian diagnostic label that followed hysteria and preceded FND. At the time, even fewer doctors understood how to manage functional symptoms, and the popular thing in care was necessarily to shrug their shoulders and send the patient home, or send them back to treatment. Maxanne felt alienated by the diagnosis, and the doctors weren’t helping; Many, of course, still don’t. “It was horrible to go through help and be treated with disdain,” she recalls. “It just cuts off your soul. And I never wanted that to happen again. Maxanne tried the treatment and even enjoyed it: it helped her start dealing with an abusive childhood. But I couldn’t see how it resembled her migraines, fatigue or tremors.
Therefore, Maxanne moved away from further therapy, and her physical condition gradually deteriorated. It was another 15 years before medicine, despite everything, began to do well.
It’s tempting to see Maxanne’s story as a representation of a frequently raised point about long covid: As public fitness professionals Steven Phillips and Michelle Williams said in the New England Journal of Medicine last year, “Our medical formula has a long history of minimizing women’s stress. “symptoms and misrepresenting or misdiagnosing their situations as psychological.
Perhaps, however, the fact is more confusing than that. In a profit-driven system, while some symptoms are minimized, others are maximized. Eli Lilly, for example, spent years commercializing the concept of excessive PMS to generate a new demand for Prozac, whose patent was about to expire. Thanks to overdiagnosis and over-remedies, 25,000 women in the United States go through an unnecessary breast cancer remedy each year, according to a recent estimate. It is widely recognized that peak C-sections are not medically necessary. And although a misdiagnosis does occur, it is arguably worse to err in exaggerated biomedicalization: for example, patients with NDF with functional seizures have been inappropriately prescribed antiepileptic drugs with serious side effects. And it’s no coincidence that Eliot Slater, the mid-century neurologist who fiercely denounced the concept of hysteria, was also one of the greatest enthusiastic proponents of the history of lobotomies.
It is annoying how statements like “dismissing women’s situations as mental” go unchallenged, as if so-called mental illnesses are frivolous or false rather than some of the persistent and irrevocable maximum reasons for human suffering. After decades of biomedical studies, we are as far from curing depression as we have long been Covid: for most patients, antidepressants slightly outperform placebos. Chronic pain has also hampered biomedicine: studies show little correlation between observable anatomical abnormalities and lived experience of pain. When suffering does not have physiological etiology transparency, it is usually more difficult to resolve. We have little about the social and curtain contexts of our lives and may not simply eliminate distress or illness even if we had more.
During the more than two centuries of medical history, some advances have reshaped the way we think about our lives. Most people can recite the definition of such discoveries: a mysterious disease killed countless people, until a drug or vaccine came along that it dramatically defeated. or tamed the disease, a story that is more or less true for syphilis, yellow fever, smallpox, measles, polio and even HIV.
For those who view disputed diseases through a biomedical lens, this story is inspiring and the need for clinical studies on cures is obvious. But style doesn’t work for all types of suffering. It is unlikely that there will ever be a penicillin for Long Covid or ME/CFS. In fact, although we have produced pills and vaccines that attack fast pathogens and make the plagues of yesteryear virtually irrelevant, we have never been very smart in treating some of our non-unusual peak chronic symptoms, such as the brain. fog, fatigue and pain. The drugs would possibly focus on a pathogen, but they’re not as smart at targeting the biopsychosocial points that shape our well-being.
Years after a global pandemic, it is terrible how medicine struggles to identify, let alone adequately treat, functional disorders or symptoms caused by psychosocial distress. In the face of such patients, the most odious doctors will drop them on a ramp in the countryside, where they will be subjected to a dubious or even damaging barrage of tests, changes, and experimental procedures rarely billable to insurance. Many others will do what they did to Maxanne in the early 2000s: pathologize them and give them back.
As she says now, Maxanne needed her illness to be socially readable. That’s why she was eternally satisfied that she was diagnosed with degenerative dementia in 2011: “I liked a terminal diagnosis that gave me a sense of dignity, and other people can check it out. “and say, ‘Oh, I’m so sorry, now I can give you my support,’ instead of ‘This is weird. ‘
But once he heard Jon Stone of Edinburgh FND, he knew that, after all, his illness wasn’t so strange: “Your brain doesn’t send or receive signals nicely from your frame,” he recalls. It works very well at the moment. But there is hope, and you are not making it up. We know this is real. But there are tactics to deal with those connections and restore the right connections.
Zachary Grin, a physical therapist who specializes in FND, told me that unlike traditional rehab with a more explicit purpose—for example, leg-strengthening exercises after a leg injury—functional symptoms require more work. systemic. to repair the connection between the brain and the body. Ask patients to count backwards through workouts by threes, or practice climbing stairs backwards, to reset their autopilot. That’s pretty much what Max and his care team tried to do, through rehab exercises, stress management, habit building, and practicing various mirror movements. Paul Garner, the UK infectious disease doctor who wrote some of the first first-person articles on the long Covid, recovered in much the same way. Both say that adopting a biopsychosocial framework has been key to their recovery and worry about how the mainstream media narrative affects patients. “I had to avoid Facebook groups, stop talking about my symptoms and try to put them in context,” Garner told me.
People like Maxanne and Paul were lucky enough to recover from the worst moments of their lives. Many other people don’t. What they had, and what each and every user with poor physical condition deserves, regardless of the cause of their symptoms, is support. They were enjoyed and supported by a circle of family members, were able not to run during their illness and had safe housing. and access to Smart Fitness Care – all the equipment they needed to thrive.
Once we finally recognize the extent to which illness is caused by psychosocial distress, we can begin to reduce its severity through policies. Redistribute resources so that no one balances your fitness at the end of your nerves. We can fund strong child care, family circle leave, and early childhood education to relieve systemic strain on women that makes them disproportionately physically fit. We can strive for universal physical care based on a number one comprehensive system of care, so that physicians and patients expand meaningful clinical relationships over time, and patients can talk about considerations and manage symptoms over time at less burdensome appointments through profit maximization.
In the meantime, we can do more to teach doctors and the public than patients like Maxanne have deserved dignity and empathy. More and more people are beginning to agree, something Maxanne felt deeply at the FND Society convention in Boston earlier this year. “20 years ago, I never imagined that so many other people would be interested in helping NDF patients,” he said. Let other people know that this happens to other people in general, to other intelligent people. brain disorder. “
Natalie Shure is a researcher in Boston. Her paintings focus on history, fitness and politics.