Health personnel across the country watched with horror as New York was the world epicenter of coronavirus. Now, as doctors in cities like Houston, Phoenix, and Miami face their own COVID-19 crisis, they turn to New York, where the number of cases has declined since then, seeking advice.
The Guardian spoke to two emergency room doctors, one in New York and the one in Houston, about what happened when COVID-19 arrived at their hospitals.
Dr. Cedric Dark, Houston: When did you start worrying about the effect of COVID-19 in New York?
Dr. Tsion Firew, New York: In February, I went to work in Sweden and Ethiopia. There was some kind of COVID-19 detection in both places. On February 22nd I arrived in New York, and nothing, without projection. At the time, I thought, “I don’t think this country is going to take good care of this.”
Dark: On February 26, in an apartment assembly, one of my colleagues put the coronavirus on the agenda. I thought, “Why do we want to worry about this here in Houston? Are you in China, are you in Europe?”
Firew: On March 1, we had our first case in New York, which at my hospital. Fast forward 15 days and I get a call that says, “Hey, you’ve been exposed to patients who are positive for COVID.” I told him to stay home.
Dark: My anxiety increased when I saw what was going on in Italy, a country I visited several times. I don’t forget to see pictures of other people dying in their homes and mass graves. I started to wonder, “Is this what we’re going to see here? Will my teammates die? Is it something my wife or I do to me, who is also an ER doctor? Are we going to take him to our son’s?”
In March, we reassigned our eight-bed emergency care unit to our coronavirus unit. And for a while, that’s enough.
Subscribe to KHN’s short morning report.
Firew: In late March, fitness staff were asked not to show symptoms returning to work. It was like a tsunami. I practiced in very low-resource environments and even in a war zone, and it may not be what I was witnessing in New York.
The emergency branch was silent, there were no visitors and the patients were very ill. Many were enthusiastic or receiving oxygen. The same human interactions as always were gone. Everyone wore a mask and dresses and there were so many other people who came here to help from other positions you didn’t know who was who. I spent a lot more time talking on the phone with my circle of family members about end-of-life care decisions, conversations you’d have face-to-face conversations.
In New York, the severity of the crisis depended on the hospital it was in. Columbia has two hospitals, one in ‘168 and one in ‘224, and the difference was day and night. The 224 is smaller and is just across the street from the Bronx Bridge, which has been hit hard by the virus.
There, other people were dying in ambulances waiting for treatment. The emergency branch brimming with oxygen-needing patients. Their corridors were filled with patients in portable oxygen tanks. We ran out of monitors and oxygen for portable tanks. Staff members succumbed to COVID-19, which aggravated the shortage of nurses and doctors.
My friends who paint in Lower Manhattan couldn’t see some of the things we saw.
Dark: I went to New York University School of Medicine and have many friends in New York with which I signed up at the time. I think in Houston, a city almost as big, we had similar crisis situations: it’s a big city with a foreign airport, it attracts a lot of business travelers and thousands of people come here every March. for the rodeo.
At the end of March, a boy my age arrived at the hospital. It was the first day we had coronavirus tests. A few days later, a nurse texted me that the patient had tested positive. He hadn’t traveled anywhere, he shows me we had a network transmission in Houston before officials admitted it.
You’ve been infected, haven’t you?
Firew: In early April, I was given in poor health with my husband. I never imagined that in 2020 I would write a living will detailing my life insurance policy to my family. Walking from my bed to the kitchen would make my center lay; I’ve wondered: will I die as my patient the other day?
A few days before I got sick, the president said anyone looking for a check could have it. But then I’m on the phone with my checkup and the Department of Health to ask for a check.
It was also at this time that a brown-skinned doctor who was about my age died of COVID-19. So I knew that being 30 wouldn’t protect me. I was even more concerned when my husband was given poor health because, as a black man, his chances of dying from this disease were much greater than mine. Or we recover, but I still have fatigue and shortness of breath.
When did the instances end in Houston?
Dark: We saw a slow build-up in April cases, however, this remained relatively quiet as the city was closed. The hospital was some kind of ghost of the town because no one had elective procedures. Things were quiet until the reopening of Texas in May.
I lost my first patient to COVID. It started crashing right in front of me. We started CPR and used the algorithms in my brain to think about how we could bring it back, but we keep coming to the same conclusion: it’s COVID and there’s nothing I can do.
It’s like serving on the front lines of a war. At first, we struggled to locate our own non-public protective apparatus while hospitals sought to protect the chain of origin. Although this scenario has stabilized, many patients who come for reasons outside COVID end up testing positive. COVID is everywhere.
Our patient population is mostly Latino-black, and for a while, our hospital has recorded one of the COVID case numbers among the nearly two dozen hospitals in the Texas Medical Center network. He revealed the flaws of a pre-existing challenge in terms of inequities in fitness care.
As domain hospitals fill up, they are reassigning more floors to COVID patients. Who knows, if we don’t do this, maybe someday the whole hospital will be COVID.
Firew: Now I’m chronically angry. Negligence came from the most sensible down. Our leaders don’t give evidence, we knew what they would do when the states reopened so quickly.
Dark: Yes, it was absolutely avoidable, if Texas Gov. Greg Abbott didn’t have to open the economy too quickly.
How’s it going in New York now?
Firew: There have been several days when I have not noticed any cases of COVID. If I see a case, it’s usually someone who’s traveled from or from other states.
People come for reasons not similar to COVID. Recently, a woman in her 40s arrived with a major chest injury. She started feeling pain three months ago, at the height of the pandemic, and was too scared to go to the hospital. To make matters worse, I didn’t have insurance and you may not have the telehealth that many had access to.
By the time he arrived at our hospital, the mass had metastasized to his spine and lungs. Even with competitive treatment, you probably only have a few months to live. This is one of the many cases we’re seeing where we’re back to “normal”: chronic disease headaches and expired cancer diagnoses. The pandemic’s burden was overtaken by a damaged physical care system.
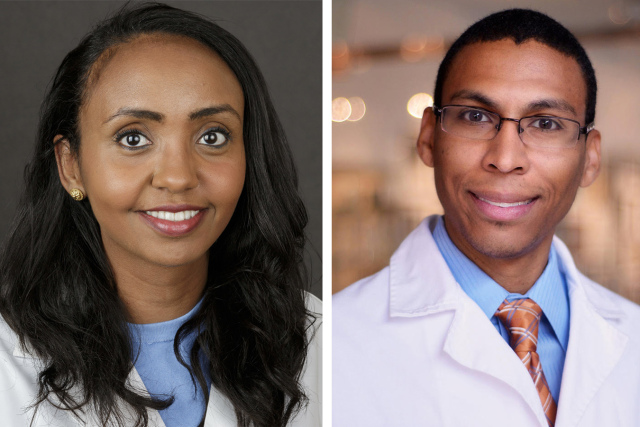
Dr. Tsion Firew is an assistant professor of emergency medicine at Columbia University and special adviser to Ethiopia’s Minister of Health.
Dr. Cedric Dark is an assistant professor of emergency medicine at Baylor College of Medicine and a board member of Doctors for America.
This verbal exchange condensed and edited through Danielle Renwick.
Share this story:
Health personnel across the country watched with horror as New York was the world epicenter of coronavirus. Now, as doctors in cities like Houston, Phoenix, and Miami face their own COVID-19 crisis, they turn to New York, where the number of cases has since declined, for advice.
The Guardian spoke to two emergency room doctors, one in New York and the one in Houston, about what happened when COVID-19 arrived at their hospitals.
Dr. Cedric Dark, Houston: When did you start worrying about the effect of COVID-19 in New York?
Dr. Tsion Firew, New York: In February, I went to work in Sweden and Ethiopia. There was some kind of COVID-19 detection in both places. On February 22nd I arrived in New York, and nothing, without projection. At the time, I thought, “I don’t think this country is going to take good care of this.”
Dark: On February 26, in an apartment assembly, one of my colleagues put the coronavirus on the agenda. I thought, “Why do we want to worry about this here in Houston? Are you in China, are you in Europe?”
Firew: On March 1, we had our first case in New York, which at my hospital. Fast forward 15 days and I get a call that says, “Hey, you’ve been exposed to patients who are positive for COVID.” I told him to stay home.
Dark: My anxiety increased when I saw what was going on in Italy, a country I visited several times. I don’t forget to see pictures of other people dying in their homes and mass graves. I started to wonder, “Is this what we’re going to see here? Will my teammates die? Is it something that happens to me or my wife, who is also an emergency doctor? Are we going to take him to our son’s?”
In March, we reassigned our eight-bed emergency care unit to our coronavirus unit. And for a while, that’s enough.
Health personnel across the country watched with horror as New York was the world epicenter of coronavirus. Now, as doctors in cities like Houston, Phoenix, and Miami face their own COVID-19 crisis, they turn to New York, where the number of cases has declined since then, seeking advice.
The Guardian spoke to two emergency room doctors, one in New York and the one in Houston, about what happened when COVID-19 arrived at their hospitals.
Dr. Cedric Dark, Houston: When did you start worrying about the effect of COVID-19 in New York?
Dr. Tsion Firew, New York: In February, I went to work in Sweden and Ethiopia. There was some kind of COVID-19 detection in both places. On February 22nd I arrived in New York, and nothing, without projection. At the time, I thought, “I don’t think this country is going to take good care of this.”
Dark: On February 26, in an apartment assembly, one of my colleagues put the coronavirus on the agenda. I thought, “Why do we want to have trouble with this here in Houston? Are you in China, are you in Europe?”
Firew: On March 1, we had our first case in New York, which at my hospital. Fast forward 15 days and I get a call that says, “Hey, you’ve been exposed to patients who are positive for COVID.” I told him to stay home.
Dark: My anxiety increased when I saw what was going on in Italy, a country I visited several times. I don’t forget to see pictures of other people dying in their homes and mass graves. I started to wonder, “Is this what we’re going to see here? Will my teammates die? Is it something that happens to me or my wife, who is also an emergency doctor? Are we going to take him to our son’s?”
In March, we reassigned our eight-bed emergency care unit to our coronavirus unit. And for a while, that’s enough.
Firew: In late March, fitness staff were asked not to show symptoms to return to work. It was like a tsunami. I practiced in very low-resource environments and even in a war zone, and it may not be what I was witnessing in New York.
The emergency branch was silent, there were no visitors and the patients were very ill. Many were enthusiastic or receiving oxygen. The same human interactions as always were gone. Everyone wore a mask and dresses and there were so many other people who came here to help from other positions you didn’t know who was who. I spent a lot more time talking on the phone with my circle of family members about end-of-life care decisions, conversations you’d have face-to-face conversations.
In New York, the severity of the crisis depended on the hospital it was in. Columbia has two hospitals, one in ‘168 and one in ‘224, and the difference was day and night. The 224 is smaller and is just across the street from the Bronx Bridge, which has been hit hard by the virus.
There, other people were dying in ambulances waiting for treatment. The emergency branch brimming with oxygen-needing patients. Their corridors were filled with patients in portable oxygen tanks. We ran out of monitors and oxygen for portable tanks. Staff members succumbed to COVID-19, which aggravated the shortage of nurses and doctors.
My friends who paint in Lower Manhattan couldn’t see some of the things we saw.
At the end of March, a boy my age arrived at the hospital. It was the first day we had coronavirus tests. A few days later, a nurse texted me that the patient had tested positive. He had not traveled anywhere; shows me that we had a network transmission in Houston before anyone admits it.
You’ve been infected, haven’t you?
Firew: In early April, I was given in poor health with my husband. I never imagined that in 2020 I would write a living will detailing my life insurance policy to my family. Walking from my bed to the kitchen would make my center lay; I’ve wondered: will I die as my patient the other day?
A few days before I got sick, the president said anyone looking for a check could have it. But then I’m on the phone with my checkup and the Department of Health to ask for a check.
It was also at this time that a brown-skinned doctor who was about my age died of COVID-19. So I knew that being 30 wouldn’t protect me. I was even more concerned when my husband was given poor health because, as a black man, his chances of dying from this disease were much greater than mine. Or we recover, but I still have fatigue and shortness of breath.
When did the résumé leave in Houston?
Dark: We saw a slow build-up in April cases, however, this remained relatively quiet as the city was closed. The hospital was some kind of ghost of the town because no one had elective procedures. Things were quiet until the reopening of Texas in May.
I lost my first patient to COVID. It started crashing right in front of me. We started CPR and used the algorithms in my brain to figure out how we could bring it back, but we keep coming to the same conclusion: it’s COVID and there’s nothing I can do.
It’s like serving on the front lines of a war. At first, we struggled to locate our own non-public protective apparatus while hospitals sought to protect the chain of origin. Although this scenario has stabilized, many patients who come for reasons outside COVID end up testing positive. COVID is everywhere.
Our patient population is mostly Latino-black and, for a time, our hospital has been ranked among the largest number of COVID cases among the nearly two dozen hospitals in the Texas Medical Center network. He revealed the flaws of a pre-existing challenge in terms of inequities in fitness care.
As domain hospitals fill up, they are reassigning more floors to COVID patients. Who knows, if we don’t do this, maybe someday the whole hospital will be COVID.
Firew: Now I’m chronically angry. Negligence came from the most sensible down. Our leaders don’t give evidence, we knew what they would do when the states reopened so quickly.
Dark: Yes, it was absolutely avoidable, if [Texas Gov. Greg Abbott] didn’t have to open the economy too fast.
How’s it going in New York now?
Firew: There have been several days when I have not noticed any cases of COVID. If I see a case, it’s usually someone who’s traveled from or from other states.
People come for reasons not similar to COVID. Recently, a woman in her 40s arrived with a major breast injury. She started feeling pain three months ago, at the height of the pandemic, and was too scared to go to the hospital. To make matters worse, I didn’t have insurance and you may not have the telehealth that many had access to.
By the time he arrived at our hospital, the mass had metastasized to his spine and lungs. Even with competitive treatment, you probably only have a few months to live. This is one of the many cases we’re seeing where we’re back to “normal”: chronic disease headaches and expired cancer diagnoses. The pandemic’s burden was overtaken by a damaged physical care system.
Dr. Tsion Firew is Assistant Professor of Emergency Medicine at Columbia University and Special Counsel to ethiopia’s Minister of Health.
Dr. Cedric Dark is an assistant professor of emergency medicine at Baylor College of Medicine and a board member of Doctors for America.
This verbal exchange condensed and edited through Danielle Renwick.
Firew: In late March, fitness staff were asked not to show symptoms returning to work. It was like a tsunami. I practiced in very low-resource environments and even in a war zone, and it may not be what I was witnessing in New York.
The emergency branch was silent, there were no visitors and the patients were very ill. Many were enthusiastic or receiving oxygen. The same human interactions as always were gone. Everyone wore a mask and dresses and there were so many other people who came here to help from other positions you didn’t know who was who. I spent a lot more time talking on the phone with my circle of family members about end-of-life care decisions, conversations you’d have face-to-face conversations.
In New York, the severity of the crisis depended on the hospital it was in. Columbia has two hospitals, one in ‘168 and one in ‘224, and the difference was day and night. The 224 is smaller and is just across the street from the Bronx Bridge, which has been hit hard by the virus.
There, other people were dying in ambulances waiting for treatment. The emergency branch brimming with oxygen-needing patients. Their corridors were full of patients in portable oxygen tanks. We ran out of monitors and oxygen for portable tanks. Staff members succumbed to COVID-19, which aggravated the shortage of nurses and doctors.
My friends who paint in Lower Manhattan couldn’t see some of the things we saw.
Dark: I went to New York University School of Medicine and have many friends in New York with which I signed up at the time. I think in Houston, a city almost this big, we had similar crisis situations: it’s a big city with a foreign airport, it attracts a lot of business travelers and thousands of people come here every March for the rodeo
At the end of March, a boy my age arrived at the hospital. It was the first day we had coronavirus tests. A few days later, a nurse texted me that the patient had tested positive. He had not traveled anywhere; shows me that we had a network transmission in Houston before anyone admits it.
You’ve been infected, haven’t you?
Firew: In early April, I was given in poor health with my husband. I never imagined that in 2020 I would write a living will detailing my life insurance policy to my family. Walking from my bed to the kitchen would make my center lay; I’ve wondered: will I die as my patient the other day?
A few days before I got sick, the president said anyone looking for a check could have it. But then I’m on the phone with my checkup and the Department of Health to ask for a check.
It was also at this time that a brown-skinned doctor who was about my age died as a result of COVID-19. So I knew that being 30 wouldn’t protect me. I was even more concerned when my husband was given poor health because, as a black man, his chances of dying from this disease were much greater than mine. Or we recover, but I still have fatigue and shortness of breath.
When did the instances end in Houston?
Dark: We saw a slow build-up in April cases, however, this remained relatively quiet as the city was closed. The hospital was some kind of ghost of the town because no one had elective procedures. Things were quiet until the reopening of Texas in May.
I lost my first patient to COVID. It started crashing right in front of me. We started CPR and used the algorithms in my brain to figure out how we could bring it back, but we keep coming to the same conclusion: it’s COVID and there’s nothing I can do.
It’s like serving on the front lines of a war. At first, we strived to locate our own non-public protective apparatus while hospitals sought to protect the chain of origin. Although this scenario has stabilized, many patients who come for reasons outside COVID end up testing positive. COVID is everywhere.
Our patient population is mostly Latino-black, and for a while, our hospital has recorded one of the COVID case numbers among the nearly two dozen hospitals in the Texas Medical Center network. He revealed the flaws of a pre-existing challenge in terms of inequities in fitness care.
As hospitals in the region fill up, they are reassigning more floors to COVID patients. Who knows, if we don’t do this, maybe someday the whole hospital will be COVID.
Firew: Now I’m chronically angry. Negligence came from the most sensible down. Our leaders don’t give evidence, we knew what they would do when the states reopened so quickly.
Dark: Yes, it was absolutely avoidable, if Texas Gov. Greg Abbott didn’t have to open the economy too quickly.
How’s it going in New York now?
Firew: There have been several days when I have not noticed any cases of COVID. If I see a case, it’s usually someone who’s traveled from or from other states.
People come for reasons not similar to COVID. Recently, a woman in her 40s arrived with a major breast injury. She started feeling pain three months ago, at the height of the pandemic, and was too scared to go to the hospital. To make matters worse, I didn’t have insurance and you may not have the telehealth that many had access to.
By the time he arrived at our hospital, the mass had metastasized to his spine and lungs. Even with competitive treatment, you probably only have a few months to live. This is one of the many cases we’re seeing where we’re back to “normal”: chronic disease headaches and expired cancer diagnoses. The pandemic’s burden was overtaken by a damaged physical care system.
Dr. Cedric Dark is an assistant professor of emergency medicine at Baylor College of Medicine and a board member of Doctors for America.
This verbal exchange condensed and edited through Danielle Renwick.
We inspire organizations to republish our content free of charge. Here’s what we asked:
You must credit us as the original publisher, with a link to our site khn.org. If possible, come with the original(s) and Kaiser Health News at the signature. Please keep the links in the story.
It is vital to note that everything in khn.org cannot be republished. If a story is classified as “All Rights Reserved”, we cannot grant permission to republish that article.
Do you have any questions? Let us know [email protected]
Thank you for your interest in supporting Kaiser Health News (KHN), the country’s premier nonprofit fitness and fitness policy writing room. We distribute our journalism without fees and advertising through media partners of all sizes and in small, giant communities. We appreciate all the participation bureaucracy of our readers and listeners, and we appreciate your support.
KHN is an editorially independent program of KFF (Kaiser Family Foundation). You can KHN by making a contribution to KFF, a nonprofit that is not related to Kaiser Permanente.
Click the button below the KFF donation page that will provide more information and FAQs. Thank you!