Editorial collaboration
Medscape
This transcript has been edited for clarity.
A recent CDC report shows that the U. S. has lost progress in treating antimicrobial resistance, largely due to the effects of the COVID-19 pandemic. In hospitals alone, antimicrobial-resistant infections and deaths increased by at least 15% in 2020 compared to 2019. Most of these infections are preventable. The CDC has many resources for physical care providers like you to help prevent those increases, patients, and maintain the effectiveness of the antibiotics and antifungals we have today.
I am Arjun Srinivasan, Deputy Director of Program Improvement in the Division of Health Care Quality Promotion at the Centers for Disease Control and Prevention. My CDC colleagues and I join their efforts to protect patients; protect fitness workers; and sell safety, quality and price in domestic and foreign fitness service delivery systems.
Many of us have worked with you on the COVID-19 pandemic and have noticed firsthand, or secondhand, not only the incredible demanding situations for patient care, but also the heroic tactics that many of you offered to care for those in need. Undoubtedly, the pandemic has brought providers, fitness services, fitness centers, and communities close to their breaking points. And while many services and systems have stabilized, we know that COVID-19 remains a major driver for the delivery of fitness services.
Thank you for your service and dedication. Thank you for your perseverance. Thank you for coming, for taking a risk to help your community, and for your willingness to serve even when we didn’t have all the answers. First of all, thank you for your patience. He has been asked to take on so many responsibilities. I’m here today to remind us of all the vital steps we can take to monitor ourselves and prevent the spread of another threat: antimicrobial resistance.
This summer, the CDC released a special on how COVID-19 has affected the nation’s progress on antimicrobial resistance.
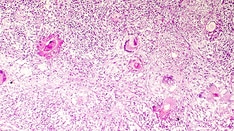
Antimicrobial resistance (or AR) occurs when organisms such as bacteria and fungi cannot be treated well with recommended agents, making them more difficult, if not impossible, to treat.
As you know, hospitals saw a very different inpatient population in 2020 than before the pandemic. Hospitals have been flooded with large numbers of sicker patients who have had longer stays and increasingly prolonged uses of invasive devices such as ventilators and catheters. The increased dangers of nosocomial infections (or HAIs) of course lead to resistance. And this, combined with points like limiting non-public protective equipment, laboratory source issues, and downsizing, would possibly have prevented physical care providers from implementing prevention methods that we know work. .
These nosocomial infections are caused by resistant pathogens such as carbapenem-resistant Acinetobacter, multidrug-resistant Pseudomonas aeruginosa, vancomycin-resistant Enterococcus (VRE), methicillin-resistant Staphylococcus aureus (MRSA), and Candida auris. 15% in 2020 compared to 2019.
This backlog is a major blow, accounting for at least 29,400 lives lost due to antimicrobial resistant infections related to physical care. The overall burden of antimicrobial resistance is likely to be much higher, but the pandemic has created knowledge gaps. In a 2021 analysis, the CDC reported pretty much the same thing: that U. S. hospitals were not allowed to do so. U. S. stocks recorded particularly high rates of 4 of the six types of hospital-acquired infections (HAIs) in the first year of the pandemic after years of stable declines. The emerging tide of hospital-acquired infections will continue to drive the progression of antimicrobial resistance unless we act urgently.
In addition to a sicker patient population and limitations in implementing infection control, CDC knowledge also shows that when COVID-19 cases are highest in hospitals in 2020, antibiotic use is also higher. , even though very few of those patients had bacterial infections. This was challenging early in the pandemic as we struggled to be more informed about control approaches and distinguish COVID-19 from community-acquired bacterial pneumonia when patients first arrived at the hospital. for evaluation
From March 2020 to October 2020, only about 80% of hospitalized COVID-19 patients obtained an antibiotic. About one-portion of hospitalized patients received ceftriaxone, which was commonly prescribed with azithromycin. We now know that many of them were not mandatory and were not to the patients who earned them.
Those of us who have the strength to prescribe antibiotics and antifungals will have to remember: as long as those drugs are used, they can contribute to the progression of resistance. Equally important, unnecessary use does not benefit the patient, but exposes him unnecessarily. to the risks of side effects such as allergic reactions, toxicity affecting organ function and Clostridioides difficile infection, which kills about 50,000 people a year.
We have learned a lot about the diagnosis and management of COVID-19 over the past 2 years, and have noticed successful approaches to antibiotic use in COVID-19 patients. Our challenge is to continue to apply what we have learned while treating patients. in the future.
The good news is that we know what works to prevent many of those infections from happening: the fundamental infections save you and the practices. In fact, from 2012 to 2017, the infections committed saved it and the efforts and increased use of antibiotics and antifungals helped decrease deaths. of antimicrobial-resistant infections in U. S. hospitalsIn the U. S. , up to nearly 30 percent. The COVID-19 pandemic has reversed some of this progress. We want to refocus our attention on protecting patients through infection prevention and improving antibiotic use while taking care of fitness.
I ask them that antimicrobial resistance was one of the most sensitive threats to the protection of our patients before the pandemic. It’s not slowing down and it’s gotten worse as we’ve focused our efforts on COVID-19. Many of you have told us about the harrowing experience of saving a COVID-19 patient only to lose them to a healthcare-related, antibiotic-resistant infection. A solution to the challenge of resistance. We want to focus on preventing infections and improving antibiotic use.
Here are 3 steps your hospital can take for patients with incurable, difficult-to-treat infections and to combat antimicrobial resistance.
First: Follow infection prevention and practices with a patient, once and both times.
This includes keeping hands blank between patients, asking patients if they recently got medical care to identify who might be at higher risk for infections, and staying informed about existing outbreaks.
Follow recommendations to avoid device- and procedure-like infections, and that environmental cleaning practices be followed for all patient parameters.
CDC also provides new infection control education for all HCP through CDC’s Project Firstline. Project Firstline provides documents you can share with your staff and colleagues so they can recognize the dangers of infection and apply movements consistently and hopefully to protect themselves. patients with hospital-acquired infections and antimicrobial resistance.
Second: how to prescribe antibiotics and antifungals.
Follow clinical and treatment guidelines.
Perform adequate diagnostic and susceptibility tests to consult antibiotic and antifungal treatment, adding appropriate medication, dose and duration.
Watch for symptoms of sepsis.
Report knowledge about antibiotic use and antimicrobial resistance to CDC’s National Health Care Safety Network and use that knowledge to indicate improvements.
Third: Encourage your patients to avoid contagion and stay informed about their vaccinations.
Vaccines delay antimicrobial resistance by preventing the spread of bacteria and reducing the use of antibiotics and antifungals.
The CDC has resources on how to be a patient safely.
Thank you for your ongoing commitment to patient safety. As Dr. Walensky, our firm principal, recently said, “Don’t forget yourself as you continue to care for others. “Our country may not have weathered the typhoon without you.
I know it will be at the forefront again as we refocus our attention on preventing antimicrobial resistance.
Thank you for listening to this insightful video observation from CDC on Medscape.
Follow CDC on Twitter
Follow Medscape on Facebook, Twitter, Instagram and YouTube
Deputy Director, Program Improvement, Division of Healthcare Quality Promotion, Centers for Disease Control and Prevention, Atlanta, Georgia Disclosure: Arjun Srinivasan, MD, disclosed any applicable monetary relationships.
You’ve already decided on My Alerts
Click on the subject below to receive emails when new items become available.