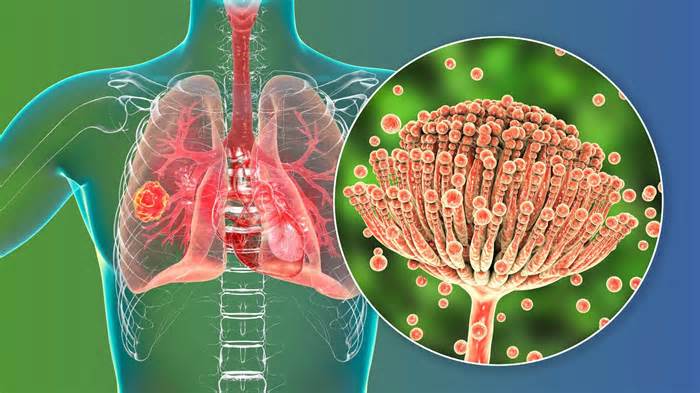
A recent study published in the Indian Journal of Critical Care Medicine presented a case series of patients with pulmonary aspergillosis (CAPA) related to coronavirus disease 2019 (COVID-19). The goal of the study is to inform doctors and health care personnel about this serious complication. similar to COVID-19.
Many radiological symptoms of COVID-19 and invasive pulmonary aspergillosis (IPA) are similar. Although API is not more unusual in immunocompromised patients, influenza infection also increases its threat in non-neutropenic patients. Respiratory viruses damage the respiratory epithelium and paralyze the local immune system. system. This damage leads to secondary and opportunistic infections, adding invasive fungal infections.
Therefore, critically ill COVID-19 patients with acute respiratory distress syndrome (ARDS) admitted to intensive care sets (ICUs) are more likely to expand CAPA. With this in the brain and the occurrence of influenza-associated aspergillosis (AAI), diagnosis of API is also necessary for COVID-19 patients. However, it is worth noting that radiology alone cannot diagnose CAPA in COVID-19 patients.
In the existing study, researchers retrospectively reviewed the medical records of all COVID-19 patients who visited Orchid Medical Center in Ranchi, India. These patients had COVID-19 shown through opposite-transcription polymerase chain reaction (RT-PCR). First, doctors prescribed a home support remedy. However, when the patient’s symptoms worsened, they requested hospitalization for further diagnosis and remedy.
High-resolution computed tomography (HRCT) scans showed cavitary lesions in the lungs of these patients. Although the effects of HRCT indicated the option of CAPA, they also performed a serum galactomannan test to improve diagnosis. The serum galactomannan test was positive for all patients. Faced with the threat of transmission and aerosolization of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), doctors have avoided bronchoscopy. Instead, they prescribed an antifungal drug, voriconazole, at a dose of 6 mg/kg every 12 hours intravenously for the first two days, followed by four mg/kg every 12 hours (maintenance dose).
Other patients in intensive care expanded APIs, and even those patients were immunocompromised. In the absence of anything else that would make those patients prone to this infection, severe COVID-19 emerged as the sole explanation for why the API progressed.
In summary, it is difficult to differentiate between fungal colonization and invasive disease without bronchoscopic sampling and microscopic evaluation of fungal cultures. The determination of galactomannan through antigen-based laboratory control supports the diagnosis of API, but a deeper technique is needed. to outline and diagnose API in COVID-19 patients. For example, tissue culture and tissue microscopy of predominantly sterile samples showing invasive expansion of septate fungal hyphae can verify the diagnosis of API. In addition, despite the threat posed by biopsies in COVID-19 patients, bronchoalveolar lavage fluid and lung biopsy are the most productive sample types for verifying the diagnosis of API in COVID-19 patients.
The existing case series has indicated an increased threat of an API emerging in critically ill COVID-19 patients, whose late diagnosis may result in increased mortality and unnecessary burden on fitness systems. Therefore, physicians deserve to look for CAPA in critically ill patients. Patients with COVID-19 who do not respond to treatment.
Written By
Neha is a virtual marketing professional founded in Gurugram, India. He holds a master’s degree from the University of Rajasthan with a specialization in Biotechnology in 2008. He has enjoyed preclinical studies as part of his assignment of studies in Toxicology Decomposition from the prestigious Central Drug Research Institute (CDRI), Lucknow, India. He also holds a certification in C programming.
Use one of the following to cite this article in your essay, article, or report:
ap
Mathur, Neha. (2022, October 14). He has rare cases of pulmonary aspergillosis related to COVID-19. Excerpt from October 22, 2022 from https://www. news-medical. net/news/20221014/Study-presents-infrequent-instances-of-COVID-19-related-lung-aspergillosis. aspx.
deputy
Mathur, Neha. ” He has rare cases of COVID-19-related pulmonary aspergillosis. “News-Medical. October 22, 2022.
Chicago
Mathur, Neha. ” He has rare cases of pulmonary aspergillosis related to COVID-19. “19-related-lung-aspergillosis. aspx. (accessed October 22, 2022).
Harvard
Mathur, Neha. 2022. Presents rare cases of pulmonary aspergillosis related to COVID-19. News-Medical, accessed October 22, 2022, https://www. news-medical. net/news/20221014/Study-presents-infrequent -instances-of-COVID-19-related-pulmonaire-aspergillosis. aspx.
News-Medical. net – An AZoNetwork website
Owned and operated through AZoNetwork, © 2000-2022