To view this article, go to My Profile, and then View Saved Stories.
To view this article, go to My Profile and then View Saved Stories.
Emily Mullin
While the first Covid-19 vaccines were released in late 2020, messenger RNA was catapulted into the public eye. Now, a few years later, interest in mRNA has skyrocketed. Clinical trials are underway for dozens of mRNA vaccines, in addition to the flu and herpes. . And scientists hope to use mRNA to treat the disease, not just save it. One of the biggest targets is cancer.
But a major obstacle is how to deliver the molecule to the place in the body that needs to be treated. Fatty bubbles called lipid nanoparticles can carry RNA into cells, and they can ferry it to a wide range of tissues but not to anywhere specific. That’s a problem for cancer, says Jake Becraft, cofounder and CEO of Boston-based Strand Therapeutics, because many cancer treatments “can be incredibly toxic in off-target tissues.” But his company may have found a solution.
Strand has figured out how to “program” mRNA much like computer code, allowing it to perform certain functions—such as turning on only in specific cell types, at specific times, and in specific amounts. Today, the biotech company announced that the US Food and Drug Administration has greenlit a clinical trial testing the approach in cancer patients with solid tumors. Strand plans to begin enrolling patients this spring. It will be the first time a programmable mRNA therapy will be tested in people.
mRNA, which is naturally provided in each and every human cell, carries the genetic blueprints needed to produce the proteins our bodies want to function. The artificial versions used in the Pfizer and Moderna Covid vaccines provide commands to create a similar coronavirus spike protein. The arm muscles recognize the spike protein as foreign and sound the alarm. The immune formula reacts and generates protective antibodies that oppose it. This way, when the body encounters the spike protein of the Covid virus itself, it is primed and able to fight off. he.
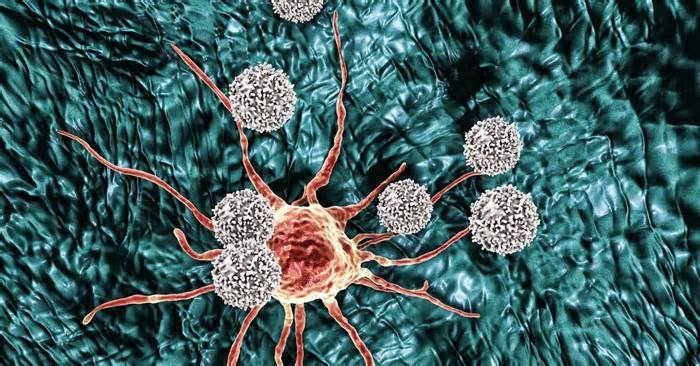
Using mRNA to treat cancer works in much the same way. Tumor cells notoriously evade the immune system, going undetected. But synthetic mRNA can direct cancerous cells to make certain proteins that alert the immune system to the tumor’s presence.
Strand’s therapy uses mRNA to make an inflammatory protein called interleukin-12, or IL-12, that causes immune cells to spring into action and unleash a cascade of events that kill cancer cells when and where they detect the protein. “What our mRNA does is go into the tumor, and then it causes that protein to be secreted by the tumor,” Becraft says. “The tumor essentially becomes a factory.”
Researchers have long thought about IL-12 as a potential cancer treatment. But in the 1990s, the first trials of IL-12 were halted when patients experienced toxic side effects. In those studies, the protein was delivered directly into the bloodstream, triggering a severe inflammatory reaction in the body. Several corporations have tried to create safer versions of IL-12, but interest from Big Pharma is waning. Last year, Bristol Myers Squibb abandoned its efforts, followed by AstraZeneca and his wife Moderna. .
Simon Hill
WIRED Staff
Dhruv Mehrotra
Rhett Allain
To fight internal tumors with IL-12, the Strand scientists designed a set of commands called genetic circuitry that tells the mRNA to produce the inflammatory protein only when it senses the tumor’s microenvironment. The circuit is designed to stumble upon grades of microRNAs, molecules that naturally express gene and emit other signatures in cancer cells compared to healthy cells. The genetic circuit tells the mRNA to self-destruct if it goes somewhere other than its intended target.
“We designed the mRNA to turn off if it goes somewhere we don’t need it,” Becraft explains.
Strand first targets easily accessible tumors, adding melanoma and breast cancer, to prove that the technique works and is safe. In this test, doctors will inject the mRNA directly into the tumors and then check how localized the effect is. In the future, Strand envisions being able to perform whole-body infusions of its programmed mRNA to treat tumors in more remote locations. The idea is that the treatment is selectively activated in certain cells and tissues.
Philip Santangelo, an mRNA researcher at Emory University’s Winship Cancer Institute, says Strand’s programmable technique has advantages, even when injected into a tumor site. “If the drug comes out of the tumor when you inject it, then at least [its effect] will be limited to the tumor,” he says.
IL-12 can be detected with certainty in the blood, so researchers will be able to take a blood pattern and make sure the protein is not present. Strand also plans to monitor the protein in the organs to see where it ends up. If treatment works as expected, they should not locate the protein anywhere outside the tumor.
But like computer circuits, genetic circuits can make mistakes, says Ron Weiss, a professor of biological engineering at MIT, co-founder of Strand and now acting as an advisor. “If your genetic circuit makes a mistake one out of 10 times, you make a mistake too. “”You don’t have to use it as therapy,” he says. If you make a mistake once every million times, that’s pretty good. “
Strand’s trial and other early attempts at these kinds of genetic circuits will see just how well they work. “The notion is that genetic circuits can really have a significant impact on safety and efficacy,” Weiss says.
Weiss pioneered the idea of genetic circuits, the first of which were based on DNA. When Becraft started graduate school in 2013, he joined Weiss’s lab to work on genetic circuits for mRNA. At the time, many scientists still doubted mRNA’s potential.
Now, Weiss imagines being able to use genetic circuits to program increasingly more sophisticated actions to create highly precise therapies. “This begins to really open up the door for creating therapies whose sophistication can match the underlying complexity of biology.”
? Get the long view on tech with Steven Levy’s Plaintext newsletter
My parents’ madness as the end of joy. Then came the robots.
Cops used DNA to wait for a suspect’s face and tried to give him facial recognition.
The planet’s aquifers are in serious trouble
We tried to create a dating app that was a chatbot to break the ice for you. It’s gotten weird.
How to Choose and Customize a Mechanical Keyboard
? Our Gear team has branched out with a new sleeping pad advisor and new selections for coolers and binoculars.
Emily Mullin
Dhruv Mehrotra
Sabrina Weiss
Tom Vanderbilt
Dhruv Mehrotra
Grace Browne
Amit Katwala
Marian McKenna
More from WIRING
Reviews & Guides
© 2024 Condé Nast. All rights reserved. Use of this site constitutes acceptance of our User Agreement, Privacy Policy, Cookie Statement, and your California privacy rights. WIRED would possibly earn a portion of sales of products purchased through our site as part of our partner component partnerships with retailers. This site may not be reproduced, distributed, transmitted, cached or otherwise used without the prior written permission of Condé Nast. Ad Choices