After the Food and Drug Administration presented dubious knowledge to justify its approval of blood plasma to treat COVID-19, some scientists are concerned that the company is trying to approve a coronavirus vaccine before it is fully tested.
On Sunday, President Donald Trump announced that the FDA had issued an emergency use authorization for blood plasma. The president, the secretary of health and human services and the head of the FDA said the remedy reduced the number of deaths among COVID-19 patients by 35%.
This is not the case and scientists questioned the FDA’s claims related to the data.
“You saw the FDA being bullied by the president of the United States to approve anything it didn’t need to pass before, because he was looking for it,” said Dr. Paul Offit, director of the Children’s Hospital’s Vaccine Education Center. in Philadelphia, in an online interview Monday with the editor of the Journal of the American Medical Association.
Knowledge showed a decrease in mortality rate in a small fraction of those who gained blood plasma, an antibody-rich fluid derived from the blood of COVID-19 survivors. Specifically, it helped others under the age of 80 who had no fan and who obtained plasma within 3 days of diagnosis.
Without a control organization of patients who didn’t get blood plasma, it’s highly unlikely to know if plasma stores lives.
The Society of Infectious Diseases of America was sufficiently involved to factor a saying that while there are “some positive signs” that plasma has helped, it does not deserve to be allowed wider use until randomized and controlled studies are conducted.
We will be in one position: the government needs a distribution formula for the COVID-19 vaccine in a position until November 1. Freezing farms and UPS are part of the plan
”I’m a scientist, a politician’: health officials respond to senators about COVID-19 vaccine
According to an unreleased study, approximately 9% of patients, younger patients, received early plasma and obtained the best doses of antibodies, died after treatment, and 12% of those who earned it later and in smaller amounts.
This is about 35% difference for this group, but that means that treatment has reduced the same number of coVID-19 deaths overall.
The FDA’s exaggeration and approval of the emergency use of the cOVID-19 remedy based on an incorrect application of an existing cure are a source of fear for scientists and vaccine-focused researchers.
They are concerned that the FDA will bend to pressure from the White House to consider an emergency use authorization, or the U.S., for a coronavirus vaccine to increase the president’s chances of re-election.
Trump said he expects a “very soon” vaccine. He raised the option that an alleged “deep-state” conspiracy at the FDA could delay it until the November 3 presidential election.
Last week, Dr. Peter Marks, who heads the FDA’s vaccination group, told Reuters that he had been stressed about launching a vaccine without sufficient protection and efficacy data. He said he’d quit if that happened.
Offit said Trump is now “trying to intimidate the FDA into approving, through an emergency use authorization, a vaccine or vaccines before they have been well tested. This is a major mistake.”
Treatment is given to people in poor health; vaccines are given to healthy people.
“Vaccines can be given to millions of others, many millions of others around the world, or even billions,” said Eric Topol, a professor of molecular medicine at the Scripps Research Institute in La Jolla, California. “How are we going to accept as true with this guy and our FDA in the coming months in connection with an emergency vaccine authorization? We are in the middle of a pandemic; there’s a lot at stake. They couldn’t be taller.”
It would possibly be sensible to grant emergency use for a COVID-19 vaccine if all knowledge of a final clinical trial showed fair protection and transparent evidence to cut the disease, and only certain “technical or administrative disorders or steps remain,” said Dr. Jesse Goodman, director of Georgetown University’s Center for Medical Product Access, Safety and Management.
If the company made this decision, the vaccine will only be used for others at increased risk of exposure to COVID-19 or the disease, he said. It would be “essential for recipients to obviously perceive that the product is not FDA approved and why and what is known and what is unknown about the protection and efficacy of the product,” he said.
More people may be if the FDA is following the procedure of fully authorizing a coronavirus vaccine rather than urgently approving it, said Daniel Salmon, director of the Institute for Vaccine Safety at the Johns Hopkins Bloomberg School of Public Health.
“It would take longer, but it could have more impact, because if other people perceive the procedure to be the general procedure and shown, it hasn’t accelerated, more people are likely to get out of it,” he said. Said.
Adoption of a vaccine without rigorous scrutiny may limit public confidence in vaccines in the coming years, said Dr. William Schaffner, a professor in vanderbilt University’s Division of Preventive Medicine and Infectious Diseases in Nashville, Tennessee.
“I can hear skeptical vaccine teams standing up and lashing out at the entire vaccine evaluation system,” he said. “That would be a profoundly bad thing for public health.”
The rush for approval can also simply recruit in vaccine studies to protect against SARS-CoV-2, the virus that causes COVID-19, as the public would possibly lose confidence in the process.
“One of the possible risks if a vaccine is released is that it would be difficult, if not impossible, for other vaccines to recruit others in their trial,” said Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases. Reuters on Monday. “The only thing you wouldn’t need to see with a vaccine is to get a U.S. before you get a sign of efficacy.”
Barry Bloom, immunologist and vaccine expert who is a professor of public aptitude at Harvard T.H. Chan School of Public Health said he had great confidence in FDA technical staff. But this is the third time in the pandemic that the FDA has made decisions more policy-based than data, he said.
The first was the issuance of an emergency authorization for hydroxychloroquine as a remedy against COVID-19 and its elimination. The timing was the FDA’s ruling to allow corporations to market antibody tests without prior approval. And now, emergency approval of the blood plasma remedy in a fragile clinical field.
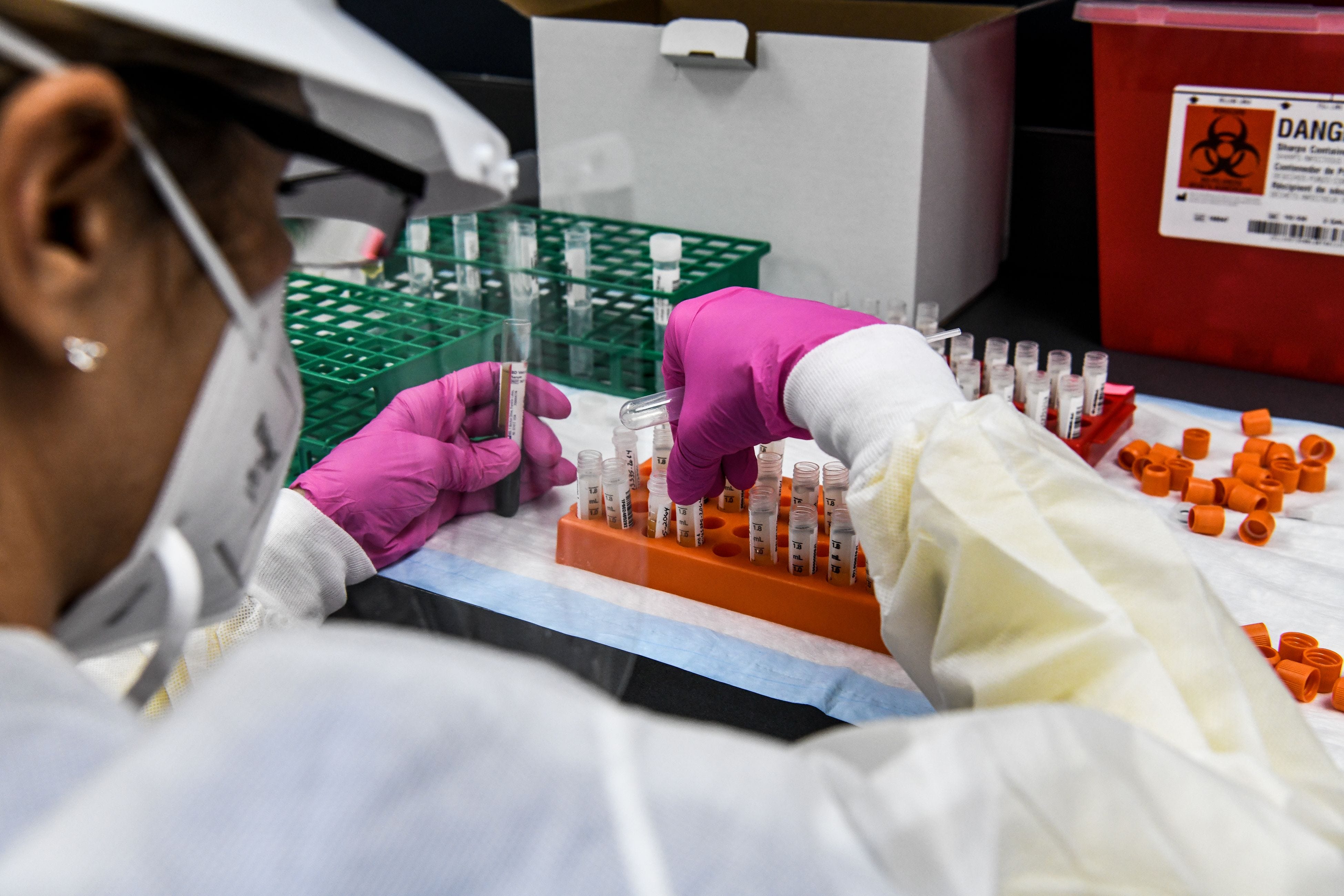
Plasma from others who have recovered from the disease contains antibodies that can help others fight the disease. The remedy has been used for more than a century against various diseases, from diphtheria in the 1890s to Ebola in 2014 and 2015.
Each disease is another and plasma can do more harm than good. That’s why careful studies are needed, Bloom said.
“I hope FDA leaders will stand firm on a clinical basis,” he said Tuesday. “Otherwise, accepting it as true across the clinical business is compromised.”
The FDA authorizes all vaccines used in the United States. At the last level of testing, called a phase 3 clinical trial, the vaccine is given to thousands of people to make sure it is effective.
When completed, knowledge is compiled into an application that is reviewed through an FDA team that includes doctors, microbiologists, chemists, biostatisticians and others.
“It’s a round-trip process” between the FDA and the company, with a lot of communication, said Norman Baylor, ceo of Biologics Consulting and former director of the FDA’s Office of Vaccine Research and Review. “The reviews are very thorough. They will have to be; are the gold standard.”
Officials have warned that they can speed up the procedure for obtaining a COVID-19 vaccine to make it public sooner and save lives.
FDA and Commissioner Stephen Hahn say corners won’t be cut. Schaffner is involved in “having left room for manoeuvre.”
He said the FDA can simply review knowledge of a giant Phase 3 clinical trial before it ends and that, based on the effects at this point, a vaccine gives the impression of being safe and effective enough to be marketed.
Phase 3 trials for the SARS-CoV-2 vaccine come with 30,000 people, of whom 15,000 get the vaccine and 15,000 get a placebo.
“It wouldn’t be great to start with the vaccine in the audience if we stopped in half, if we only had another 7,500 people who won the vaccine,” Schaffner said.
It takes time to see if there are protection problems among thousands of volunteers and judge whether they are due to an infection, Topol said.
Despite Trump’s repeated statements that a vaccine will soon arrive, there has been no time for this knowledge to become available.
“There is no meaningful knowledge this year, period,” Topol said. All that happens so temporarily is “a hoax.”