In the first wave of COVID-19, the purpose of the tests is to have a broad look, locate hidden cases and have an idea, says Dr. Gerald Evans of Queen’s University, “how widespread the infection is in our society. “
The consistent results have led provinces like Ontario to increase the number of tests from a paltry 5,000 per day to get a better picture of the virus and the number of “susceptibles” that remained among us.
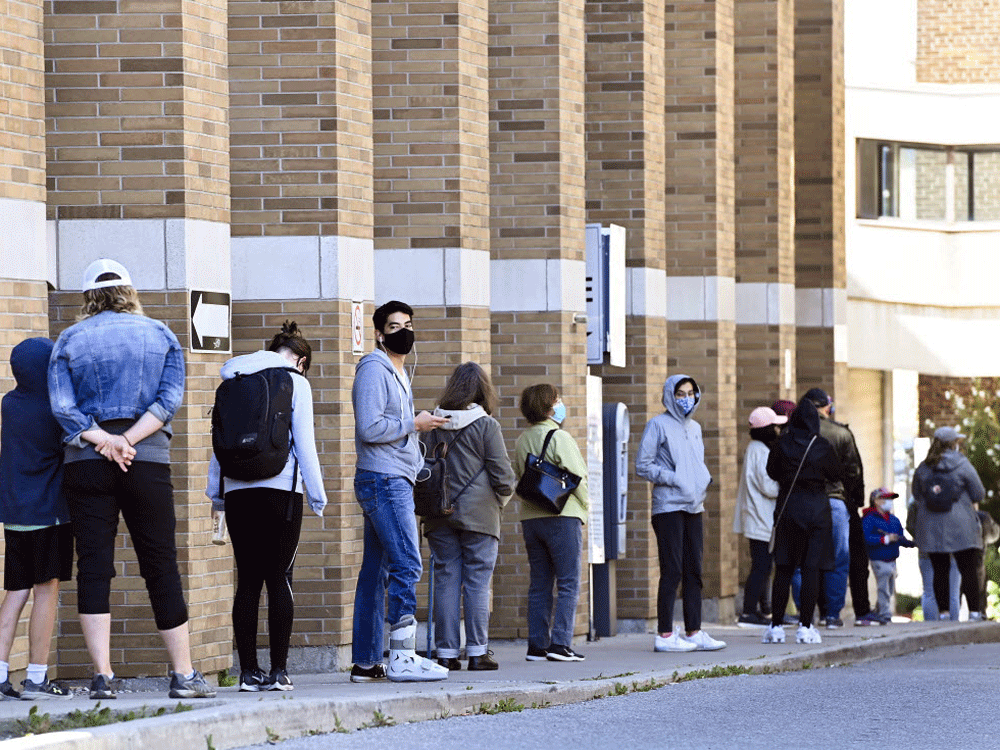
Alberta and Ontario opened shortly after selection for those looking to get tested, even if they had no known symptoms or had no contact with a shown case— the same people who are now requesting overloaded pandemic testing systems.
Alberta announced Thursday that the reset button is urgent, temporarily stopping asymptomatic tests in anticipation of a decrease in the call for tests as schools reopen and bloodless flu viruses and reach the year.
Since 29 May, Alberta has conducted some 233,000 tests on others who had no symptoms, of which only 0. 07% produced positive results, about 163 cases. Alberta evaluated an average of another 13,625 people per day for more than seven days, nearly six times the other 2,380 people who took the tests coincided with the day of March and April. About $74.
Canada’s laboratories tested an average of 47,111 more people according to the day during the following week, of which 1. 4 with the percentage were positive.
Ontario will soon get “a few thousand” of new COVID-19 testing centers in pharmacies for others without symptoms, Prime Minister Doug Ford announced this week. The concept is to reduce congestion at COVID evaluation sites. The province will accentuate the evidence like never before. Previously,” Promised Ford. Ontario has increased its capacity from the earliest days, from 5,000 to 25,000 to 30,000 tests consistent with the day, with plans to build up to 50,000 consistent with day and beyond.
But Evans and other experts say that, if necessary, Ontario deserves to start evaluating others who have no known symptoms or known contact. The concentrate deserves to be in the immediate diagnosis of others with symptoms. Evans and others are less interested, in asymptomatic and risk-free contact with other people, “because they provide less data at this level of the pandemic, and we know that many other people with bloodless symptoms provide evidence, and we want to be able to locate those who are genuine COVID so that we can find them with tactile search and isolation. »
Evans, president of Queen’s Infectious Diseases Department, said the public was excited that asymptomatic COVIDS accounted for 40% of infections. “We know that’s probably not true,” Evans said, other truly asymptomatic people with COVID-19 are well below 20%, Evans says, “probably in the 10-15% diversity of all cases. “
People without symptoms who have still been socially active are much more likely to be HIV positive. “The user who has no symptoms and who has been intelligent, without direct contact, the probability that we will discover that it is positive will be extremely low. “, Evans says, at a rate of about less than 1%.
Part of the challenge is the feedback cycle: the instances shown are increasing, the media reports that the number of instances is increasing, others are concerned, and they start appearing in discovery centers.
In addition to anxiety, young people return to school and public fitness standards are set to ensure that each and every child who coughs or has a possible symptom of COVID is sent home and controlled, all of which results in mass traffic in control centers. , and with the opening of thousands of new control sites in Ontario for asymptomatic controls, the challenge remains to have enough laboratory capacity to process them.
If the new sites still have to use the same methods, the same nasal smear samples, the same molecular tests that are to be done in centralized laboratories, “you will face the same disorders in terms of response times, laboratory capacity, machines lack reagents,” says Dr. Zain Chagla, infectious disease doctor and associate professor at McMaster University in Hamilton. Ontario.
Until rapid and affordable testing is passed through a federal government that does not seem in a hurry to do so, priority will be given to others with symptoms and those who have been particularly exposed, according to experts. “By flooding the asymptomatic test system, we are committing this reaction,” says Dr. Dominik Mertz, an infectious disease specialist at McMaster University. The more bottlenecks there are, the longer the processing times of the results, the longer the reaction time to a positive test.
Alberta will continue to offer asymptomatic testing to high-risk groups, adding physical care workers, teachers and staff, others living in long-term care services, and homeless people.
Dr. Bonnie Henry, a fitness worker in the province of British Columbia, has withstood the evidence of others without known symptoms or known contacts, arguing that the evidence does not prove it.
Some say we want to reduce the concentration on daily numbers. The existing reference swab test used to trip over viral RNA, a sticky molecule, can remain positive for weeks after infection, which does not necessarily mean the user is contagious.
The user who has no symptoms that has been wellArray . . . the probability that we’ll find out it’s positive will be incredibly low
Dr. Irfan Dhalla should place more emphasis on the number of cases with unknown source of transmission, the proportion of tests performed in less than 24 hours, and the number of contacts known on the day and contacted within 24 hours of identification. , the source of exposure is “unknown” in about 40% of cases, “so it is transparent that the test, suggestion and isolation formula is not running as well as it could,” says Dhalla of Unity Health Toronto.
However, the number of social contacts a 20-year-old can have in just 3 days is huge, Evans says. And as more cases arise, we overcome the ability of public fitness to seek contacts. “Here we are talking about thousands of other people who want to be tracked. It’s still an old archaic formula of a phone and a list, which lists names. “
While cases are declining, deaths and hospitalizations remain low. During the summer, COVID-19 entered younger and less at-risk age groups, where it is intensifying. “If you stayed in that age group, it would be great,” says University of Toronto epidemiologist Dr. David Fisman. “The challenge is that this will be the case, and we have noticed that this trend is reproducing now, again and again, in France, Spain, Florida, Austria.
“One of COVID’s wonderful tragedies is our inability to be informed from elsewhere. “
– With the Calgary Herald
Email: skirkey@postmedia. com Twitter: sharon_kirkey
Sign up for news from the National Post, a department of Postmedia Network Inc.
An error has occurred, provide a valid email address.
A welcome email is on the way. If you don’t see it, check your unwanted folder.
The next factor in the newsletter will soon be in your inbox.
We found a challenge when you signed up. Check again
Postmedia is committed to maintaining a still civil discussion forum and encouraging all readers to express their views in percentage on our articles. Comments can take up to an hour to moderate before appearing on the site. We ask that you keep your comments applicable and respectful. I’ve enabled email notifications. You will now receive an email if you get a reaction to your comment, an update to a comment thread that follows, or if a user follows it. Check out our network regulations for more data and main points on how to adjust your email settings.
365 Bloor Street East, Toronto, Ontario, M4W 3L4
© 2020 National Post, a department of Postmedia Network Inc. All Rights Reserved. Unauthorized dissemination, transmission or transmission is strictly prohibited.
This uses cookies to personalize your content (including ads) and allows us to analyze our traffic. Learn more about cookies here. By using our site, you agree to our terms of use and our privacy policy.