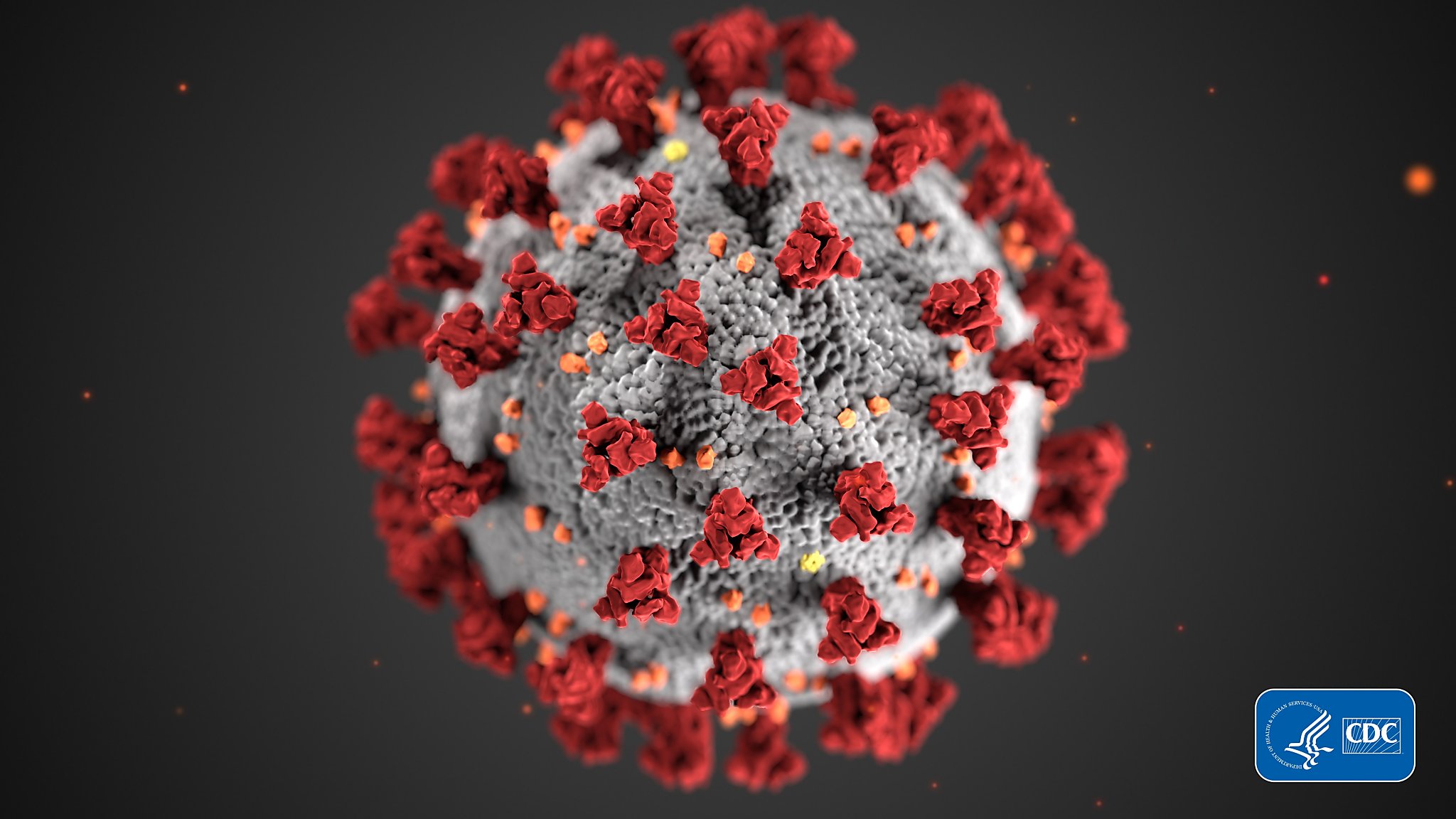
This illustration, created at the Centers for Disease Control and Prevention (CDC), shows the ultrastructural morphology exposed through coronaviruses.
One of the complicated facets of COVID-19 is that other inflamed people seem to suffer from a wide variety of other diseases. The virus can wreak havoc on one patient’s gastrointestinal system, while causing shortness of breath and fever in another.
While cough, fever and odor loss are known as the 3 key symptoms of COVID-19, researchers used the knowledge of a symptom monitoring app with more than four million users to identify a long list of additional symptoms, adding headache, muscle pain and fatigue. , diarrhea, confusion, loss of appetite, shortness of breath and more.
Focusing on a subset of the knowledge of approximately 1,600 COVID-19-infected users in the UK and US, the team learned the six symptom teams described below:
1. Flu without fever: headache, loss of smell, muscle pain, cough, sore throat, chest pain, no fever.
2. Flu with fever: headache, loss of smell, cough, sore throat, hoarseness, fever, loss of appetite.
3. Digestive system: headache, loss of smell, loss of appetite, diarrhea, sore throat, chest pain, no cough.
4. Severe level 1, fatigue: headache, loss of smell, cough, fever, hoarseness, chest pain, fatigue.
6. Severe and respiratory level 3: headache, loss of smell, loss of appetite, cough, fever, hoarseness, sore throat, chest pain, fatigue, confusion, muscle pain, shortness of breath, diarrhea, pain.
The researchers then conducted deeper research to determine whether others on specific symptom teams had a more serious illness and were more likely to need respiratory assistance.
They found that 1.5% of patients in the first organization, 4.4% at the time and 3.3% in the 3rd organization want respiratory assistance. These figures were 8.6%, 9.9% and 19.8% for groups 3, 4 and 6, respectively. In addition, almost part of the patients in organization 6 ended up in the hospital, at only 16% of those in the first.
The team then developed a style that matched patients’ age, sex, BMI and pre-existing situations, as well as symptoms collected five days after the onset of the disease. He predicted which organization a patient belongs to and their threat to require hospitalization and respiratory assistance more than an existing threat style based only on age, sex, BMI, and pre-existing situations.
“If you can expect who these other people are on the fifth day, you have time to provide them with early interventions, such as tracking oxygen and blood sugar levels, and making sure they are well hydrated, undeniable care that can be given. at home, avoiding hospitalizations and saving lives,” Steves said.
Dr. John Swartzberg, a professor of infectious diseases and vaccines at UC Berkeley, said studies have the potential for doctors and other physical care providers to identify others who will require prior intervention and more physically.
“Certainly, we’ll have to see how it’s painted in the ‘real world,'” said Swartzberg, a COVID-19 expert who didn’t paint in the studio. “With widespread use, it deserves ” to learn “and gradually more effective”.
MORE CORONAVIRUS COVERAGE:
Register here to receive the “The Daily” letter about the latest coronavirus.
– Can collective immunity prevent coronavirus? What we know now: is it less harmful to reopening elementary schools than the best? – The Bay Area reflects the COVID-19 ‘stabilization’ trend of the rest of the state – the undeniable way to create an effective polypropylene cleaning for your mask – Can you contract a coronavirus twice? Doctors aren’t sure even when anecdotal reports accumulate
Amy Graff is the editor-in-chief of SFGATE. Write to him: [email protected].