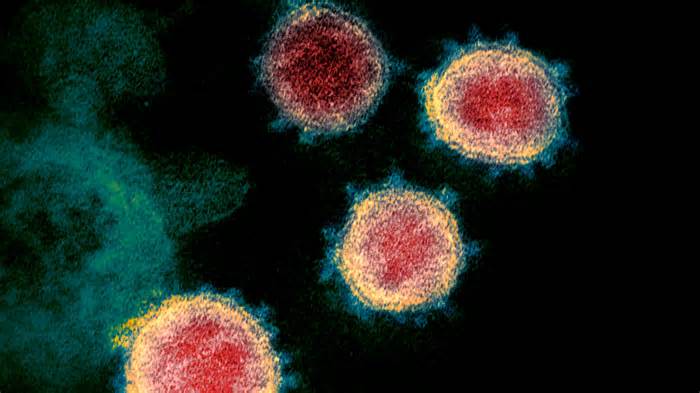
When the coronavirus emerged, a mystery emerged: Why did some inflamed people never develop the symptoms?
A more likely explanation is that they are possibly a person’s lucky genes.
A new study published Wednesday in the scientific journal Nature suggests that other people with an express edit of a gene were more likely to experience an asymptomatic infection than those without.
The applicable gene set is as human leukocyte antigen or HLA.
“This is the first time that, in a rigorous and physically powerful way, someone has shown that there is a transparent and definitive genetic basis for asymptomatic [coronavirus] disease, not all asymptomatic diseases, but a subset of other people who remain asymptomatic,” said Jill Hollenbach, a professor of neurology at UC San Francisco, who co-authored the study.
Hollenbach and other researchers recruited about 30,000 more people for the study, all of whom already had genetic data recorded because they had registered as potential bone marrow donors with the National Marrow Donor Program.
The scientists asked those other people to sign up for the COVID-19 citizen science study, organized through UC San Francisco researchers, and use a smartphone app to track the effects of coronavirus testing and any symptoms.
The researchers had a significant pattern of coronavirus-positive patients of European ancestry to generate meaningful data; There were too few positive participants from other ancestors for those effects to be significant.
Scientists knew of another 1,400 people of European descent who tested positive for coronavirus in the first year of the pandemic, and not all were vaccinated because no vaccines were yet available.
Of this group, 136 were asymptomatic, or about 10%. The reasons other people without symptoms were tested may be due to the nature of their job, such as being a health care employee undergoing regime testing, or perhaps a family member became inflamed and exposed to the virus.
Significantly, the scientists found that other people who had an edit of the gene called HLA-B*15:01 were more than twice as likely to remain asymptomatic as those without, Hollenbach said.
And if a user had two copies of the edit of that gene, one parent, “was 8. 5 times more likely to remain asymptomatic,” Hollenbach said.
“I’ve been worried about those HLA disease distribution studies my entire career, and we’ve actually been pretty stunned. It was a strong effect,” he said.
The findings add to smaller studies that genetics were potentially linked to asymptomatic coronavirus infection.
Just to make sure what they were seeing was real and not something specific about their specific study organization, the scientists also reanalyzed data from a UK cohort and conducted genetic research from another patient organization studied by other researchers at UC San Francisco.
“We were able to reflect that same finding,” Hollenbach said. At the time, we were convinced it was a genuine effect. “
The new study also suggests why this specific edit of this gene might have helped some of the ravages of the worst pandemic in fashion history.
One of the reasons the coronavirus is so fatal is that it’s new. Since it had not yet circulated, other people had not been exposed and many lacked immunity to fight it.
But for other people with this special edition of this gene, the study suggests that their immune systems were better able to attack the pandemic coronavirus, officially known as SARS-CoV-2.
And the explanation of why this?
After past skirmishes with other common, non-pandemic coronaviruses, the culprits of the common bloodlessness, other people with this edit of this gene have developed the equipment to better protect themselves against the pandemic strain of coronavirus that began spreading in late 2019. There are four seasonal coronavirus strains that are generally responsible for 15-30% of respiratory tract infections during the year.
Other scientists have warned in the past that other people would possibly have had some degree of immunity to SARS-CoV-2 due to previous reports of their body with seasonal coronaviruses. But with this study, scientists have taken the concept to another level.
To make this determination, the study authors took samples of T cells, a vital component of the body’s immune formula, that had been collected years before the pandemic began and turned them into pieces of SARS-CoV-2 in the lab. Lab data show that T cells from other people with this component edit of the HLA gene should recognize those pieces of SARS-CoV-2 and respond protectively.
“People with this B*15:01, for some reason, some of them have this pre-existing immunity after exposure to seasonal bloodless viruses that turns out to be remarkably effective in fighting the virus” that explains COVID-19, Hollenbach said.
Having that gene editing “is the key to having this very pre-existing immunity,” he added.
Hollenbach said studies are underway to conduct studies in particular for other people of non-European descent.
The study does not suggest that B*15:01 is the only explanation for why some other people were asymptomatic. Further studies would possibly find other factors, adding non-genetic factors.
“But for some reason, past immunity mediated by B*15:01 is effective and gives other people the possibility of becoming inflamed with SARS-CoV-2 without having any symptoms,” Hollenbach said.
He has more than 3 dozen co-authors, with contributions from scientists around the world, plus Australia and Britain. In the United States, contributions came from other scientists at UC San Francisco, the University of North Carolina at Charlotte, and the University of Utah, as well as the Center for International Blood and Marrow Transplant Research and the National Marrow Donor Program.