As Covid-19 rose five years ago, no one knew what to expect.
Neither did the immune system.
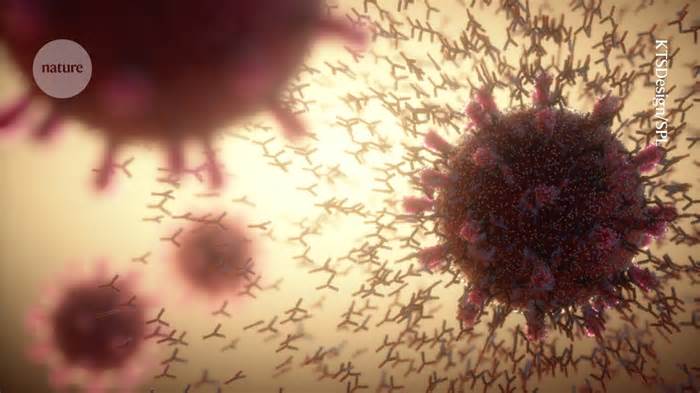
Confronted with a new virus, humanity was immunologically naive. The emergence of SARS-CoV-2 provided a rare opportunity to study the immune system in action, and researchers raced to gather all the data they could. “The world was exposed to a brand-new pathogen,” says Nadia Roan, an immunologist at the University of California, San Francisco. “We were trying to leverage that to learn more about immunity.”
Years later, scientists are still sifting through the data to garner a better understanding of how the immune system works. Here are four lessons they’ve learnt so far.
Early in the pandemic, many researchers focused on the antibodies produced in response to SARS-CoV-2 infection. Like antibodies, the immune components called T cells also combat infection — but these drew less attention at first. Many clinical trials of COVID-19 vaccines, for example, analysed antibody levels and not T cells.
This is partly due to the fact that T cells are more difficult to examine than antibodies, and our understanding of them was delayed, explains Shane Crotty, an immunologist at the Jolla Institute of Immunology in San Diego, California Aterray
As the pandemic continued, it has become transparent that the T cells were an arm of the reaction to the Sars-Cov-2 and COVVI-19 vaccines, explains Alessandro Satede, also an immunologist at the Institute of Immunology of Jolla. Antibodies opposed to SRAS-COV-2 decreased in the months after vaccination, but other vaccinated people continued to make T cells that identified the virus1. This coverage of the T lymphocytes remained strong, Settete and others discovered 2, even opposed to the viral variants that dodged the antibody defenses raised through the first generation of tin vaccines.
“People went more to antibodies and tended to the responses of T cells,” said Rosemary Boyton, an immunologist at Imperial College in London. “Now we perceive a lot, much greater than T -cell responses are also important. “
The pandemic also gave researchers new insights into the innate immune system, another line of defence against viruses.
Innate immune reactions are not as express as antibodies and mobile T. Cells can release those reactions when they stumble upon strange molecules, such as RNA Sars-COV-2 When a mobile discovers a revealing molecule, it raises the alarm, releasing proteins called interferons. These proteins are activated by gene loads, many of which are worried in viral defense. The interferon reaction also alerts other mobiles in the same organ to be on alert, says Benjamin Tenoever, a virologist from the University of New York in New New York. “It can be very overwhelming for a virus. “
Children and Covid: Why Young Immune Systems Are on Top
Before the pandemic, researchers thought that this warning cry did not travel far beyond the site of infection. But when tenOever and his colleagues analysed samples from hamsters and from autopsies of people who had previously been infected with SARS-CoV-2, they found signs of interferon responses throughout the body, even in organs far away from infected cells3. Later, the team learnt that this is not limited to SARS-CoV-2: the flu virus also elicits a widespread interferon response in hamsters.
The faint mortgage that these global antiviral defenses decorate coverage in case the infection moves through the body. It can also be a component of the explanation why the SARS-COV-2 variants that propagate later in the pandemic are less probably that their predecessors cause serious illness: the subsequent variants joined more than the previous bureaucracy of the virus to the cells to the cells of the nose, keeping the virus in the upper breathing tract longer. This allowed the innate caution sign to succeed in the lungs and strengthen the defenses there before the virus arrived.
Before the pandemic, researchers weren’t very interested in the nose, explains José Ordovas-Montanes, an immunologist at Boston Children’s Hospital in Massachusetts. “He thought of it as an undeniable passive tube to bring air to the lungs,” he said. “And the lungs were the position where the company happened. “
The pandemic underscored the importance of understanding immune responses in specific tissues, and especially in the place where infection often starts: the nose.
The rainy lining of the nose is an exclusive immune environment that another combination of antibodies and immune cells that discovered it in the blood. As a result, injected vaccines, which generate antibodies in the bloodstream, possibly would not be ideal for blocking nose infection. “One of the pandemic classes is the location, the location, the location,” says Crotty.
Doi: https://doi. org/10. 1038/d41586-025-00128-W