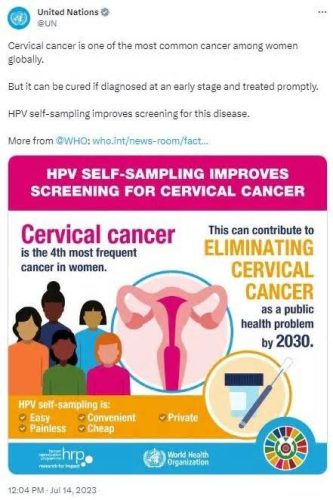
Cervical cancer is the fourth most common cancer in women globally, with an estimated 604,000 new cases and 342,000 deaths worldwide.
Few diseases have global disparities as distinct as cervical cancer. Nearly 90% of deaths in 2020 occurred in low- and middle-income countries, which face delays in immunization, testing and treatment.
In August 2020, the Global Strategy for the Elimination of Cervical Cancer was approved by the World Health Assembly.
To achieve them by 2030, WHO has instituted global targets classified 90-70-90: to ensure a final rate of 90% HPV vaccination among women up to the age of 15; examine 70 per cent of women between the ages of 35 and 45; and provide treatment to 90% of women diagnosed with cervical disease.
To achieve those ambitions, BGI Genomics has released a comprehensive global report on cervical cancer awareness.
The objective of this report is to assess knowledge, attitudes, and practices similar to cervical cancer screening and HPV vaccination. By examining those critical areas, this survey seeks to highlight the obstacles and opportunities that accompany them.
The extensive survey covers 1,878 women from various regions, including Brazil, mainland China, Saudi Arabia, Serbia, Thailand and Uruguay. The findings highlighted the pressing need to remove barriers, raise awareness and access to testing and immunization services.
HPV awareness affects cervical cancer screening rates: Globally, 40. 0% of women did not know that HPV is responsible for more than 95% of cervical cancer cases. Among those who were unaware of the link between HPV and cervical cancer, 39. 1% had abstained from cervical cancer. screening, exceeding the global average of 31. 2%.
More choices, fewer barriers: Among women younger than 25, HPV prevalence peaks at 22%. However, 43. 5% of women surveyed in the 21-25 age group, the highest percentage among the groups, were reluctant to ask a male doctor for an appointment. This highlights the desire to give women, especially younger women, the opportunity to undergo HPV DNA testing along with Pap tests.
Vaccination and screening form a virtuous circle: cervical cancer screening was performed in 82. 1% of vaccinated women, compared with 60. 6% of unvaccinated women. HPV vaccine was administered to 45. 8% of women screened and 22. 1% of women not screened. those who have missed national vaccination programs, places and times of detection.
Early detection of cervical cancer is imperative to save lives and ultimately eliminate this dreaded disease, according to WHO’s global strategy. This study shows that raising awareness among women could be the missing link to increasing vaccination and screening rates.
Early diagnosis and activation therapy are imperative to cure cervical cancer. For women in the general population, WHO recommends starting screening at age 30 and routinely testing for HPV every five to ten years.
HIV-positive women deserve to be tested more (every 3 to 5 years) because they are six times more likely to develop cervical cancer.
Globally, 40. 0% of people are unaware that HPV is responsible for more than 95% of cervical cancer cases. In particular, Saudi Arabia (51. 2%) and Thailand (47. 3%) have the highest levels of awareness of this fact.
In addition, 31. 2% of the rest of the people worldwide have never been screened for cervical cancer. Among women who are unaware of the link between HPV and cervical cancer, 39. 1% have never been screened for cervical cancer, exceeding the global average.
Specifically, Saudi Arabia (55. 8%) and Serbia (36. 5%) have the percentages of women who have never been screened for cervical cancer. This gap highlights a lack of awareness that influences cervical cancer detection rates.
Internationally, knowledge about Pap smears (81. 0%) is twice that of HPV DNA testing (38. 9%). When it comes to Pap tests, Serbia (95. 1%) and Brazil (91. 1%) have degrees of knowledge, while mainland China (64. 8%) and Thailand (50. 5%) lead HPV DNA testing.
In addition, after knowing its greater accuracy (95% accuracy rate), 88. 0% of Americans worldwide are more susceptible to HPV DNA testing than to Pap smears (with an accuracy diversity of 80-90%). Mainland China (92. 3%) and Thailand (94. 0%) have the highest percentages of people who prefer HPV DNA testing.
As for the knowledge of HPV as a sexually transmitted virus, 77. 9% of Americans worldwide know it. Knowledge is lowest in Saudi Arabia (55. 3%) and mainland China (72. 9%).
Lack of symptoms (42. 3%), worry about the effects (40. 7%), and humiliation of seeing a male doctor for a Pap smear (39. 0%) are the main barriers to cervical cancer screening.
The countries with revisions in this regard are Uruguay (55. 9%), Brazil (51. 1%), mainland China (59. 4%) and Saudi Arabia (44. 9%), all involved in the lack of symptoms.
In Saudi Arabia (51. 9%) and mainland China (57. 1%), there is a strong reluctance to have a male doctor administer a Pap test. Among older people aged 21 to 25, the oldest group among the age groups surveyed, 43. 5 in agreement with percent expressed doubts for this reason.
In contrast, physician referral (75. 9%) is women’s primary motivation for cervical cancer screening. Points based on behavior, such as new sexual partners or the detection of a lack of sexual monogamy in your partner, rank particularly low, at 25. 5%. reported on symptoms and behavioral points to provide informed recommendations.
WHO has expressed alarming fears about a widespread decline in global HPV vaccination policy due to the effect of COVID-19.
Between 2019 and 2021, the first-dose HPV vaccination policy decreased significantly, from 25% to 15%. As a result, 3. 5 million more women were not vaccinated against HPV in 2021 compared to 2019. To oppose this downward trend, countries want to step up efforts for HPV vaccination programs.
The main disincentive for women to get vaccinated against cervical cancer is the lack of knowledge about where to get vaccinated (38. 7%). This was followed by a narrow absence of symptoms (36. 8%) and concern about side effects (28. 6%). such as Thailand (50. 8%) and Serbia (49. 5%) have the highest percentages of people who do not know the places of vaccination.
The HPV vaccine is given to 38. 4% of women worldwide. However, the percentages are much lower in Saudi Arabia (29. 5%) and Serbia (7. 8%). In particular, 46. 0% of women between the ages of 21 and 25 have been vaccinated against HPV, which is higher than the global average.
HPV vaccines should be given before HPV exposure and sexual activity for optimal results. WHO recommends vaccinating women aged nine to 14 years to gain increased coverage against cervical cancer and proposes an exact vaccination schedule in its December 2022 position paper.
As for the wisdom of age diversity through the WHO (9 to 14 years) to initiate vaccination, only 43. 2% of international Americans have this wisdom. Countries such as Saudi Arabia (20. 8%) and Thailand (25. 4%) have the lowest rates of awareness. of this age group.
Only 17. 9% of the world’s population knows the vaccination schedule by age group, such as two doses six months apart for women over 21 years of age. Brazil (10. 2%) and Serbia (14. 0%) are the least familiar with this applicable vaccination schedule. .
WHO stresses that a coordinated cervical cancer prevention strategy should include educating Americans about cutting behaviors that increase the risk of HPV infection, as well as disseminating data on screening, vaccination, diagnosis, and treatment of precancerous lesions, cancer, and risk factors.
The HPV vaccine serves as the number one preventive measure and does not require screening later in life. Current vaccines do not offer coverage unlike all high-risk HPV types and have limited influence on disease in unvaccinated women and those who were vaccinated at an older age. centuries.
Among those who won the HPV vaccine, 82. 1% also underwent cervical cancer screening, well above the average for unvaccinated organizations of 60. 6%. This trend is much more pronounced in Thailand, where 97. 7% of immunized women opted for screening compared to 61. 4%. % of women not immune. Image credit: BGI Genomics
Since not all women were vaccinated before screening, the study also looked at whether those who opted for screening were more likely to be vaccinated. women not examined.
BGI Genomics, headquartered in Shenzhen, China, is one of the world’s leading providers of embedded precision medicine solutions. In July 2017, it became a subsidiary of BGI Group and is officially listed as BGI Genomics (300676. SZ) on the Shenzhen Stock Exchange. .
The CE-certified SENTIS™ HPV test fuses self-sampling generation and genotyping verification to find the 14 most critical “high risk” HPV types, which come with HPV-16, 18, 31, 33, 35, 39, 45. , 51, 52, 56, 58, 59, 66 and 68, as well as 2 types of “low risk” viruses, HPV -6 and 11.
With next-generation sequencing (NGS) technology based on a large volume of sample for analysis, HPV genotyping detection reduces the burden of testing based on the individual. In 2021, the WHO approved DNA testing as the number one screening method for cervical cancer prevention.
This study is based on an online survey of 1,878 participants from Brazil (315), mainland China (310), Saudi Arabia (312), Serbia (307), Thailand (319) and Uruguay (315).
These participants resided in their respective countries or regions at the time of the survey in July 2023. Conducted in local languages, the age of respondents ranged from 21 to forty-five years. The survey was conducted through Momentive Global under commission.
BGI Genomics is the world’s leading provider of embedded precision medicine solutions and now serves consumers in more than one hundred countries.
They provide educational institutions, pharmaceutical companies, healthcare providers and other organizations with embedded genomic sequencing, proteomic services, clinical services and answers in a wide variety of applications.
They have more than 20 years of genomics experience and help their customers and partners achieve their goals by delivering fast, high-quality effects employing a wide diversity of cutting-edge, cost-effective technologies, adding their own state-of-the-art DNBSEQ ™ sequencing. technology.
Sponsored Content Policy: News-Medical. net publish articles and similar content that would likely come from resources with which we have existing business relationships, provided that such content adds price to News-Medical. Net’s core editorial philosophy of educating and informing the site. Visitors interested in medical research, science, devices and medical treatments.
Use one of the following to cite this article in your essay, article, or report:
. APPLICATION
BGI Genomics. (2023, August 15). Empowering Women’s Health: BGI Genomics Global Cervical Cancer Awareness Report 2023. Retrieved August 23, 2023, https://www. news-medical. net/whitepaper/20230815/Empowering-Womens-Health-BGI-Genomics-Global-2023- Awareness-report on-cervical-cervical cancer. aspx.
deputy
BGI Genomics. ” Women’s Health Empowerment: BGI Genomics Global 2023 Cervical Cancer Awareness Report. News-Medical. August 23, 2023.
Chicago
BGI Genomics. ” Women’s Health Empowerment: BGI Genomics Global 2023 Cervical Cancer Awareness Report. News-Medical. https://www. news-medical. net/whitepaper/20230815/Empowering-Womens-Health-BGI-Genomics-Global- 2023-State-of-Cervical-Cancer-Awareness-Report. aspx. (accessed August 23, 2023).
Harvard
Genomics BGI. 2023. Empowering Women’s Health: BGI Genomics Global Cervical Cancer Status Awareness Report 2023. News-Medical, accessed 23 August 2023, https://www. news-medical. net/whitepaper/20230815/Empowering-Womens-Health -BGI-Genomics-Global-2023-State-of-Cervical-Cancer-Awareness-Report . aspx.
News-Medical. net – An AZoNetwork website
Owned and operated through AZoNetwork, © 2000-2023