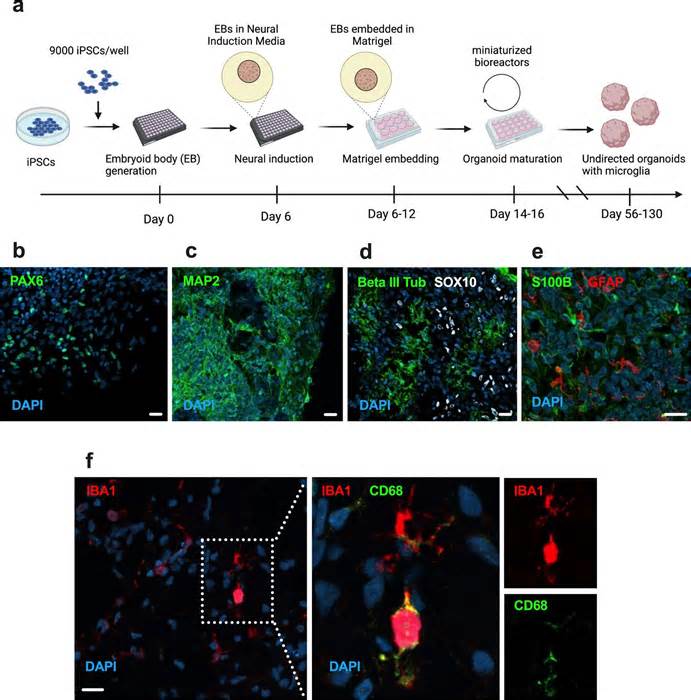
Several studies reported persistent cognitive symptoms after COVID-19 infection, but the underlying mechanisms remain unknown. The researchers of the study, published as a quick communication in the journal Molecular Psychiatry, created three-dimensional styles of the brain in a dish, called brain organoids, of human-induced pluripotent stem cells (iPS). The style differs from previous ones because the researchers also included the brain’s immune cells, microglia.
In inflamed styles, microglia excessively engulfed synaptic structures and showed positive regulation of points involved in phagocytosis. The style evolved and the effects of the study can only consult long-term efforts to address cognitive symptoms in the wake of COVID-19 and other neuroinvasive viral infections.
Cognitive deficits after infection
“Interestingly, our effects largely mimic what has recently been observed in mouse models inflamed with other neuroinvasive RNA viruses such as West Nile virus. These viruses are also connected with residual cognitive deficits after infection and persistent microglia activation. Superior absorption from synapses, which has been recommended to cause those symptoms. Several studies have now also reported cognitive symptoms remaining after COVID-19 infection, as well as an increased threat of being diagnosed with a disorder characterized by cognitive symptoms,” says Samudyata, a postdoctoral fellow in the Sellgren Laboratory in the Department of Physiology and Pharmacology at Karolinska Institutet.
Links to Parkinson’s and Alzheimer’s
Microglia are the brain’s resident immune cells, but they also play vital roles in regulating neural circuits in the adult and developing brain. Exaggerated swallowing of synapses has been linked to neurodevelopmental disorders, such as schizophrenia, as well as neurodegenerative disorders, in addition to Alzheimer’s disease.
By sequencing genes on individual mobiles, the authors also had to examine how other types of mobile phones responded to the virus.
“Microglia showed a distinct genetic signature, largely characterized by upregulation of interferon-sensitive genes, and included pathways in the past connected to neurodegenerative disorders such as Parkinson’s disease and Alzheimer’s disease. This signature was also observed at a later time when viral load was minimal,” says exam co-author Susmita Malwade, a PhD student at the Sellgren Laboratory in the Department of Physiology and Pharmacology at Karolinska Institutet.
Please indicate the appropriate maximum category to facilitate the processing of your request
Thank you for taking the time to provide feedback to the editors.
Your opinion is for us. However, we do not guarantee individual responses due to the large volume of messages.