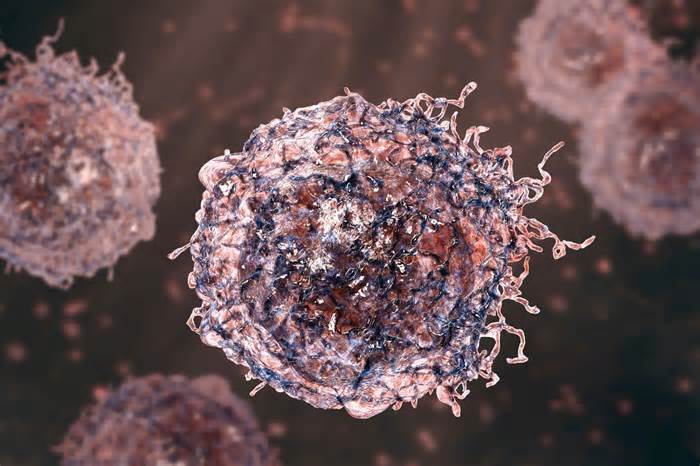
In a recent clinical letter published by the Brazilian Society of Dermatology, researchers highlight the prospective role of severe acute respiratory syndrome coronavirus 2 infections (SARS-CoV-2) in triggering the relapse of mycosis fungoides, a form of cutaneous T-cell lymphoma.
The authors aimed to talk about a report describing the recurrence of mycosis fungoides in a patient after contracting coronavirus disease 2019 (COVID-19). They described the symptoms and tests that showed COVID-19 and the recurrence of mycosis fungoides and talked about viral prospective. mechanisms that may cause immune dysregulation in patients with cutaneous T-cell lymphoma.
The authors described the case of a 60-year-old patient with mycosis fungoides, whose cancer was controlled with ultraviolet A and 8-methoxypsoralen phototherapy, followed by narrowband ultraviolet B therapy. He became inflamed with SARS-CoV-2 through family contact and developed a maculopapular rash.
At two weeks, pruritus was observed in spaces with erythema, and the papules peeled and flattened. At two months, the papules in the patient’s extremities, stomach and trunk were transformed into parchment plaques.
SARS-CoV-2 was shown through a positive immunofluorescence test. D-dimer values were maximum (1876 ng/mL) and well above the positive threshold (>500 ng/mL). Normal x-ray.
Histopathology showed motile atypia and lymphocyte exocytosis, and immunohistochemistry decreased CD7 T cells and CD4 T cell elevation, indicating level IB motile cutaneous T lymphomas.
The authors discussed immune dysregulation related to SARS-CoV-2 infections that can potentially pose the threat of cutaneous IB T-cell lymphomas such as Sézary syndrome and mycosis fungoides. Although the environmental and infectious triggers of cutaneous T-cell lymphomas have been well reported explored, theories of the pathogenesis of mycosis fungoides and Sézary syndrome come with upregulation of helper T (Th) cells type 2 and reduction of Th1 cells, as well as secretion of cytokines such as interferon α and interleukin-12.
COVID-19 has been linked to unbalanced cytokine production, downregulation of regulatory mobile T activity, and increased serum D-dimer and C-reactive protein levels. In addition, SARS-CoV-2 infections are thought to increase the production of autoantibodies, exacerbating or triggering autoinflammatory and autoimmune diseases such as Kawasaki disease, Guillain-Barré syndrome, immune thrombocytopenic purpura and most likely systemic sclerosis and lupus erythematosus.
Although controlled cutaneous T-cell lymphomas are not inherently a threat to COVID-19, competitive cutaneous T-cell lymphomas, immunosuppressive treatment to treat those lymphomas, patient complex age, and lymphopenia would likely increase the threat of infection and severity of COVID-19.
To conclude, this letter highlights a case of recurrent cutaneous T-cell lymphoma after SARS-CoV-2 infection in a 60-year-old patient. The authors symptom and immunological tests showed COVID-19 and recurrence of mycosis fungoides.
The letter discussed other autoimmune and autoinflammatory diseases known to have been triggered or exacerbated by COVID-19 in genetically predisposed individuals. The case highlighted the need to perceive immunogenetic dysregulation related to SARS-CoV-2 infections to mitigate the possible recurrence of cutaneous T. -cell lymphomas and other cancers in patients with controlled or indolent cancers.
Written By
Chinta Sidharthan is a Bangalore-based India. Su academic background is in evolutionary biology and genetics, and has extensive experience in clinical studies, teaching, clinical writing and herpetology. Chinta holds a PhD in evolutionary biology from the Indian Institute of Science and is passionate about science education, writing, animals, wildlife and conservation. For his doctoral studies, he explored the origins and diversification of blind snakes in India, where he conducted extensive fieldwork in the jungles of southern India. He has won the Governor General Bronze Medal and Gold Medal for Academic Excellence award from the University of Bangalore and has published his studies in high-impact journals.
Use one of the following to cite this article in your essay, article, or report:
ap
Sidharthan, Chinta. (2022, Oct. 17). Could COVID-19 infections cause a relapse of mycosis fungoides or cutaneous T-cell lymphomas?Retrieved October 27, 2022, from https://www. news-medical. net/news/20221017/Could-COVID-19-infections-cause-a-relapse-of-mycosis-fungoid-or–cutaneous-T-cell-lymphomas. aspx.
deputy
Sidharthan, Chinta. ” Could COVID-19 infections cause a relapse of mycosis fungoides or cutaneous T-cell lymphomas?”News-Medical. October 27, 2022.
Chicago
Sidharthan, Chinta. ” Could COVID-19 infections cause a relapse of mycosis fungoides or cutaneous T-cell lymphomas?”News-Medical. https://www. news-medical. net/news/20221017/Could-COVID-19- infections cause a relapse of mycosis fungoides or cutaneous T-cell lymphomas. aspx (accessed October 27, 2022).
Harvard
Sidharthan, Chinta. 2022. Could COVID-19 infections cause a relapse of mycosis fungoides or cutaneous T-cell lymphomas?/Could COVID-19 infections cause a relapse of mycosis-fungoid-or–cutaneous-T-cell-lymphomas. aspx.
News-Medical. net – An AZoNetwork site
Owned and operated through AZoNetwork, © 2000-2022