Bonsoir. I’m Karen Kaplan, and it’s Tuesday, August 16th. Here’s the latest news on what’s happening with the coronavirus in California and beyond.
In December, when South Africa took stock of the first global increase in COVID-19 driven through the Omicron variant, fitness experts were pleasantly surprised by what they saw.
In Gauteng Province, new infections have equaled the record in the past set through Delta, and have done so much faster, thanks to Omicron’s unprecedented ability to spread. But the new variant caused much less damage along the way.
The threat of hospitalization in inflamed adults was 29% lower than in previous outbreaks, and the chances of being admitted to an intensive care unit also decreased. Pieter Streicher, a coronavirus analyst at the University of Johannesburg, predicted that hospitalizations would end. being 25 times lower than would be expected for such a high infection rate.
Even better: Across the country, the death rate among other people who contracted the coronavirus dropped dramatically in this first wave of Omicron.
Observations like those were repeated around the world as Omicron crossed borders and oceans with shocking efficiency. It wasn’t long before Omicron earned a reputation as a softer edition of SARS-CoV-2.
Now, as lawmakers and other ordinary people wonder if it’s time to avoid altering our lives to avoid infection, some scientists point to an inconvenient truth: We still don’t know if Omicron is softer than its predecessors.
We know that Omicron caused less damage. But that may say more about the situations in which Omicron arrived on the scene than the homes intrinsic to the virus itself.
“It’s widely said that Omicron is inherently less pathogenic, but there’s no genuine evidence of that,” Dr. Christopher Chiu, a COVID-19 researcher at Imperial College London, told my colleague Melissa Healy.
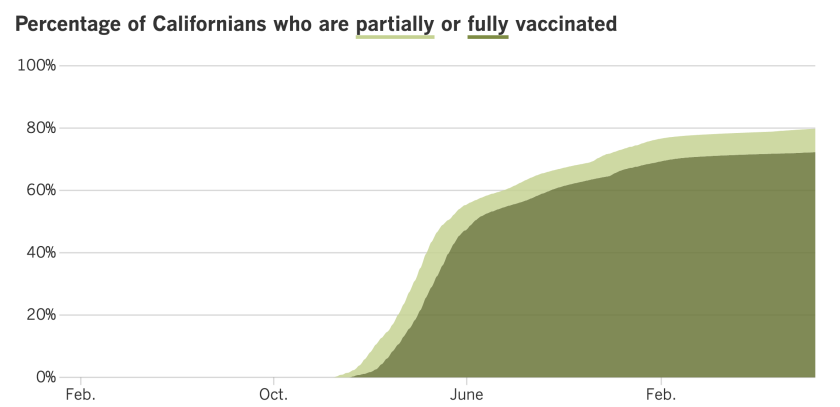
When Omicron arrived on U. S. shores. right after Thanksgiving, Americans had a really extensive point of immunity. Sixty percent of us had been fully vaccinated and about a third were immune to a previous infection. (These teams overlapped, but it’s unclear to what extent. )
In addition, those who were inflamed anyway benefited from remedies that were not had in past outbreaks caused by the original Wuhan strain or the Alpha and Delta variants it generated.
If Delta had arrived in those conditions, perhaps it would have sweets too.
“Comparisons to Delta are like apples and oranges,” Chiu said. “Delta was circulating at a time when many were not yet vaccinated or were already infected. In contrast, Omicron largely causes advanced infections in other people who already have partial coverage opposite to the vaccine. “Induced immunity or infection.
Trying to what extent Omicron’s benevolence is due to its inherent characteristics is not easy. A study published in the journal Nature found that in petri dishes, Omicron attacked upper respiratory formula cells with less enthusiasm than Delta. Omicron was also much less able to infect lung tissue and other cells of the lower respiratory tract.
Other studies conducted on animals such as hamsters and mice found that creatures inflamed with Omicron lost less weight than those inflamed with Delta. This is telling, because the more serious an infection, the greater the weight loss. Animal studies have also shown that Omicron causes less inflammation in the lungs.
An ideal way to find out if Omicron is inherently less harmful would be to gather other people who have won the same number of doses of vaccines and past infections, and then intentionally infect them with other versions of the virus and see how they fare.
If this kind of study sounds familiar, it’s because Chiu did one like this in London to see what the original strain of the coronavirus was doing to the body. It is now making plans for a follow-up trial that would use Delta and Omicron. The effects may provide a clearer picture of whether Omicron is less difficult for its victims.
The answer matters. If it turns out that Omicron’s reputation for walking lightly is justified, we can remember our pandemic precautions with confidence. On the other hand, if Omicron is as virulent as his predecessors, we might have to remain a little more on guard.
“That’s a question,” said Dr. Stanley Perlman, a virologist at the University of Iowa and a leading coronavirus expert. The genuine picture is “unclear. “
Cases and deaths in California at 2:50 p. m. Tuesday:
Follow the progress of the coronavirus in California and vaccination efforts, adding the most recent numbers and their breakdown, with our charts.
My colleague Gustavo Arellano puts on a lot of hats. He’s the host of The Times, our podcast about news and culture. He is a regular columnist for Californie. He is successful with writing the Essential California newsletter.
Apparently, this was not enough to keep you completely busy. He recently called Los Angeles County Public Health Director Barbara Ferrer to offer hers for another mission: the COVID-19 good luck story.
Arellano is part of the shrinking minority of Americans who are still virgins of the coronavirus. Not only has he moved away from the hypercontagionous variant of Omicron and its various subvariants, but as far as he knows, he has not been inflamed with any edition of the coronavirus since the beginning of the pandemic.
“I think I’m special, someone worthy of a case study,” Arellano wrote.
It is not known how giant this organization is. But with an average of about 95,000 new infections in the U. S. In the U. S. over the past week, the lines of those who never flared are shrinking throughout the day.
A report led by researchers from the Centers for Disease Control and Prevention’s COVID-19 Response Team estimated that 58% of U. S. citizens became inflamed at least once in February. This figure was based on an ongoing study that analyzes blood samples sent to clinical laboratories to see if they involve antibodies that are only produced in reaction to a coronavirus infection. (Samples from other people suspected of COVID-19 are excluded from the investigation so as not to distort the results. )
By mid-July, near the peak of the BA. 5 outbreak, the percentage of Americans who had at least one coronavirus infection had risen to 82%, according to models developed at the University of Washington’s Institute for Health Metrics and Evaluation. .
Arellano has noticed that the number of uninfected people is reduced in his own social circles. Among his relatives, he is now the only one who has no direct experience with the virus. (This is even though everyone is fully vaccinated. )and doubly enhanced. )
This counts as an achievement in my book. But in Ferrer’s pro-opinion, that didn’t make Arellano an anomaly enough to justify turning it into a kind of case study.
“I’m not surprised,” he told Arellano after learning of his condition. “There are still a few million people in Los Angeles County who haven’t contracted it yet. “
Ferrer’s assessment that Arellano had benefited from luck and perhaps also from intelligent genes.
“We’ve been in such a fight over the mask, but most of the people who told me they hadn’t won COVID tell me they were dressed in a mask,” Ferrer said.
Arellano admitted that he first and foremost resisted masks. He used one for his homework, but not when he wasn’t on time.
“I found them silly and embarrassed to use one. He highlighted my forehead, you know?” he said. When he covered himself, he opted for a bandana.
It was his wife, Delilah Snell, who convinced him to change his habits. Thanks to his insistence, Arellano switched to a cloth mask, then to a surgical mask and then to a high-quality N95 “which I now wear as comfortably as a windbreaker. “” he said.
Snell is the owner of the Alta Baja market in Santa Ana. Arellano wrote that consumers at the cheerful boutique and bistro should wear masks unless they are sitting and eating.
It’s hard to miss the message: Last summer, as the Delta variant increased, at least five symptoms about the mask policy were posted at market gateways. The front.
There are no exceptions for spouses.
“What changed me was that my wife told me that I would be barred from her store if it was not prudent,” Arellano wrote.
This vigilance has paid off: Snell is a coronavirus virgin.
In her opinion, there is nothing confusing about this, there is no explanation as to why scientists need her or her husband.
“Wear a mask!” Snell intervened when Arellano spoke with Ferrer. “This pandemic would have been gone a long time ago if other people just wore their masks!”
Ferrer the comment.
“Your wife has been right from the beginning,” he said. “Listen to her more. She has the wisdom of women who care for others.
Discover the advances in vaccination in California with our tracker.
Congratulations, Los Angeles County! You have officially downgraded your COVID-19 level.
The CDC’s most recent assessment took Los Angeles out of the “high” category and the “medium” category. The federal firm said Thursday that the county’s coronavirus case rate over the past week was about 302, consistent with 100,000 residents, which is considered high. But the number of newly hospitalized patients with coronavirus infections in the past week rose from 10. 1 to 9. 9 consistent with 100,000 people, according to the CDC. Falling below 10 is the key to moving from “high” to “medium” territory.
County fitness officials unofficially withdrew from the “high” category on July 28. On that date, the CDC stated that Los Angeles had 10. 7 newly hospitalized coronavirus-positive patients consistent with a population of 100,000 in the past week. But Ferrer said that was based on his department’s recent high figures, the real number 9. 7. (This statistic saved the county a new inner mask mandate. )
According to a Times investigation of county data, the average number of new infections reported per day decreased 23% week over week, to just 263 new cases per 100,000 citizens per week. That’s more than 302 per 100,000 people.
“Because viral transmission remains high, there are still thousands of new people every day who become inflamed and can infect others,” Ferrer said.
And yet, look, it turns out that more and more people are willing to let go of their infection prevention routines. Cdc is looking to keep them in the game with new rules that simplify its latest advice.
Very little is different in the new directives. Getting vaccinated and strengthened as soon as you’re eligible remains the most sensible thing on the list, as is the advice to get tested if you think you might be infected. However, the widespread test to detect giant populations of other asymptomatic people is now only for other people living in high-risk settings, such as nursing homes and prisons. The same goes for contact tracing (although those efforts have already been scaled back).
Those who test positive are asked to self-isolate for at least five full days and only come out of isolation after their COVID-19 symptoms have increased and they have not had a fever without taking medication for at least 24 hours. The firm stands by its controversial position that a negative coronavirus check is not mandatory to end isolation.
But now he says a role to play if other people don’t need to continue wearing a mask until the end of their tenth day: If you mark negative on day 6 or later, then recheck negative 48 hours after that, you’re loose to give up your mask, according to the CDC.
Some other people deserve to plan for self-isolation for at least 10 full days, adding those who have experienced shortness of breath or other breathing problems, patients who have required treatment in the hospital, and other immunocompromised people. But the new rules minimize the desire to quarantine if you’ve been exposed to someone who is inflamed but hasn’t tested positive yourself. Instead, you deserve to wear a high-quality mask when you’re with other people (in case you end up with an infection) and check yourself at least five days after exposure to see if you’re inflamed.
The Food and Drug Administration (FDA) has issued its own guidance on coronavirus verification. Instead of performing two rapid antigen checks to make sure you’re not infected, the FDA now says it needs three. The update is partly about the effects of a government The study found that adding a third test to nutrition significantly improved the accuracy of the effects.
Drug regulators in the UK are the first in the world to approve a new edition of Moderna’s COVID-19 vaccine that targets the Omicron variant in addition to the original coronavirus strain. The combination vaccine will be presented to others 50 years of age and older. as reinforcement, according to the Regulatory Agency for Medicines and Medical Care.
Moderna and Pfizer are using “bivalent” COVID-19 vaccines for the U. S. market. But the British vaccine is a little different: the edition of Omicron that is designed to recognize is BA. 1, while the vaccines are ready for the United States. Will pass after subvariants BA. 4 and BA. 5. The CDC’s most recent estimates are that those two strains account for more than 94% of the SARS-CoV-2 coronaviruses circulating here.
And finally, this week’s list of COVID-19 celebrities includes First Lady Jill Biden (who has mild symptoms), Secretary of Defense Lloyd J. Austin III (who had already had the first outbreak of COVID-19 Omicron in January), and Pfizer CEO Albert Bourla (who won 4 doses of his company’s Comirnaty vaccine and now takes his Paxlovid antiviral tablet).
Today’s consultation comes from readers who need to know: how can my child COVID-19 be in school?
Whether your child is starting kindergarten or entering their senior year of high school, just spending hours in study halls with dozens of other students is bound to result in exposure to the coronavirus at some point. (One of my son’s classmates brought the virus with him on the first day of school. )
But exposure doesn’t have to lead to an infection, and the American Academy of Pediatrics has this recommendation to keep young children safe:
• Make sure your student is vaccinated against COVID-19. Keeping up with vaccines is “the most effective way for children,” Dr. Brown said. Sonja O’Leary, who chairs the academy’s School Health Council. Anyone who is at least 6 months old is eligible for a COVID-19 vaccine, and children five years of age and older could be eligible for a booster.
• Consider wearing a mask inside the school. Even if it’s not mandatory, it’s still helpful, especially for students who are unvaccinated, immunocompromised, whose family member is at risk of becoming seriously ill, or who live in a county with a higher COVID-19 network point. A mask that fits well around the nose and mouth is preferable.
• Remind students to wash their hands thoroughly. This is especially important before eating.
• Keep young people at home if they are sick.
If sending your child back to school makes you a little nervous, you may feel reassured knowing that the academy says the risks are manageable and valuable.
“One of the most important classes of the pandemic is that children are more likely to learn, thrive and grow well when they attend school alongside their peers,” the AAP said in a statement.
We need to hear from you. Email us with your coronavirus inquiries and we will do our best to respond to them. Wondering if your query has already been answered? Check out our archives here.
Backpack? Verify.
Bottle of water? Verify.
Mask? Verify.
The students pictured above, Isabella Sosa, 5, and her brother Daniel Sosa, four, chose to start their new school year at Vena Avenue Elementary School in Arleta with colorful masks on their faces. It’s just a sign of the times.
The siblings were among about 437,000 students from the Los Angeles Unified School District who introduced a new year monday.
It is the third first day of school in the district since the beginning of the pandemic. Parents and educators said they expected campus life to be almost general this time around.
“I’m thrilled that my son is learning,” Donovan Donaldson, a father at Plummer Elementary in the North Hills.
The students were also impatient, and he added Haley Henderson, a junior at King/Drew Magnet High School of Medicine and Science in Willowbrook, who still dreams of spending her entire freshman year at home. “I’m excited to be here,” she said. So I think it fills that void. “
To follow
Karen Kaplan is a science and medical editor at the Los Angeles Times. Before joining the Panel, he worked in the Business section. He graduated from MIT and Columbia University.
Subscribe to access
To follow