Good night. I’m Karen Kaplan and it’s Tuesday, January 17. Here’s the latest news on what’s happening with the coronavirus in California and beyond.
It’s been over 3 years since the pandemic began, and there’s still a lot left that has researchers scratching their heads. The most sensible thing on this list is the long COVID.
The condition is so misunderstood that there is no agreed definition of what it is. Nor does it have a universally accepted name. ” Long COVID” is the one we see most often, but others come with long-term COVID, chronic COVID, and the PASC medical center moniker (which can mean post-acute COVID-19 sequelae or post-acute sequelae of SARS-CoV-2 infections).
Prolonged COVID is characterized by a number of fitness disorders that can last for months. In some cases, symptoms persisted for a year or more. The more severe a COVID-19 patient’s initial war, the greater the COVID threat. However, it can also be triggered through asymptomatic coronavirus infection, meaning other people can contract prolonged COVID without knowing they’ve had COVID-19.
The government’s current definition of prolonged COVID EE. UU. de states that symptoms present at least 4 weeks after “the initial phase of infection. “The number and type of symptoms can vary greatly from user to user, making the condition difficult to understand.
Luckily for us, an organization of researchers in Israel conducted a study of thousands of COVID-19 patients and the large number of symptoms documented in their medical records. As my colleague Corinne Purtill reports, the study team focused on other people with mild cases. of COVID-19, unlike those who were in poor enough health to be admitted to the hospital.
Each of the nearly 300,000 people who tested positive for coronavirus infection matched some other user of the same age, sex and vaccination status. Both members of a pair also shared a similar set of pre-existing conditions, such as diabetes or immunodeficiency. disorders. The main difference is that the paired “controls” had not tested positive for coronavirus infection.
The researchers compared the medical records of each inflamed user and their non-inflamed counterpart over a 12-month period. This allowed the team to assess the threat of long-term COVID symptoms arising and see how long they tended to last. The findings were published last week in the medical journal BMJ.
The bad news is that even other people with mild COVID-19 are at higher risk for long-term COVID symptoms. The most productive news is that the list of symptoms is small and most disappear within a year.
For example, among the 76% of study subjects who were not vaccinated against COVID-19 when researchers began following them (mainly because vaccines were not yet available), those who had tested positive for coronavirus infection in the first place faced a greater threat. of having a persistent cough than their peers who tested negative. But within 4 months, the threat to other people on either team was the same.
Hair loss, a common physical manifestation of acute stress, was more likely to affect other people who tested positive than those who tested negative, but the main threat lasted no more than seven months. The trend was the same with central palpitations and chest pain, it took 8 months for threats to be equalized in both groups.
There were a handful of symptoms that would likely haunt other people after an entire year. 19 patients twice as many as their non-inflamed peers. However, this is an improvement over the six-month mark, when previous patients were 5 1/2 times more likely to enjoy a loss of smell or taste.
Other symptoms that were more likely for COVID-19 survivors one year after infection were shortness of breath, weakness, and memory and concentration disorders.
The researchers said both men and women were equally likely to see prolonged COVID symptoms within a year.
If you’re the type to drink half full, those effects are worth reassuring. Prolonged symptoms of COVID can have a huge effect on quality of life, and months go by slowly when you’re debilitated, but at least you know that. in the vast majority of cases, those symptoms will have disappeared by the first anniversary of the infection.
Still, advocates for long-standing COVID patients remind us that there are no promises when it comes to recovery.
“There are a number of patients who have a very long-term chronic illness, who are now living 3 years of unrelenting illness,” said Lauren Stiles, Long COVID Alliance executive committee member.
Case and in California at 5:30 p. m. Tuesday:
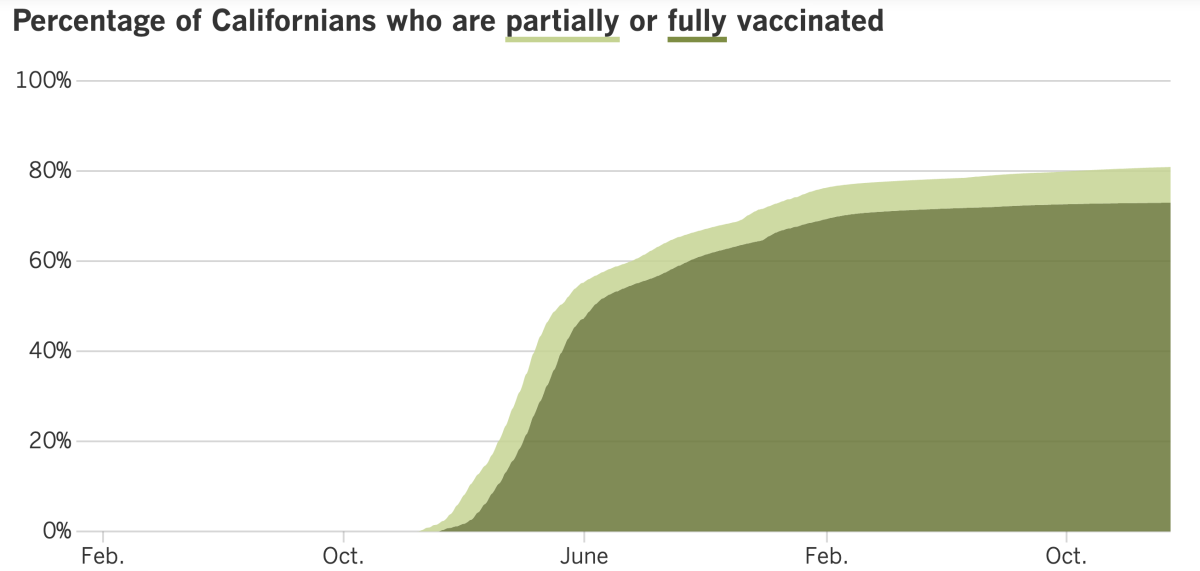
Track California’s coronavirus and vaccination efforts, adding the latest numbers and their breakdown, with our charts.
If you’re still running from home, relying on Amazon and Instacart to deliver parts you used to buy in person, and streaming videos on Netflix from watching them in the theater, you’re missing out on a vital kind of social interaction.
Yes, it is imperative to keep in touch with close friends and family circle members, the other people with whom we have “strong ties,” in sociology. Dozens of studies have documented the benefits of having a strong social network. Researchers say it’s as healthy as quitting smoking.
It turns out that there is also merit in having “relational diversity. “This means having types of interactions with people.
Here’s an example of a day with relational diversity: Start by sharing breakfast with your spouse. On the way to work, he stops for coffee and chats with the barista. Her time at the workplace includes conversations with colleagues and calls a friend to catch up while traveling at night. Once you get home, briefly greet neighbors as you walk your dog, then head to your monthly poker group meeting.
A conservative COVID user who is still semi-isolated may have as many interactions a day, but will most likely focus on a small organization of family, colleagues, and close friends.
Hanne Collins is a graduate student who reads organizational habits at Harvard University. Their studies found that the more social interactions a user has overall, the greater their well-being. In addition, Collins found that the diversity of those social interactions is also a predictor of a user’s well-being. In fact, social diversity is a greater predictor of well-being than if a user gets married.
These effects suggest that it is incumbent on all of us to interact in conversations with others we don’t know very well, such as the barista and neighbors.
“We’re not saying weak ties are that strong, but our loved ones [friends and family] are all around us; we’ve incorporated them into our lives,” Collins told my colleague Deborah Netburn. make the other connections happen. “
A generation ago, before we could use smartphones to order takeout delivered via a robot and receive our recipes, dry cleaning, and other essentials at our doors, we still had no option to interact with strangers. Now it’s the kind of thing that makes other people uncomfortable, said Nicholas Epley, a professor of behavioral science at the University of Chicago’s Booth School of Business.
Epley’s studies have shown that other people tend to underestimate the emotion they can derive from a verbal exchange with a stranger. For example, he asked other people who took the bus or exercised to paint if they expected how much they would like to communicate. to some other traveler instead of being alone. Most respondents expected to be happier alone, but they were wrong: communicating with a stranger brought forward their trip.
If this makes you think about tactics to spend more time talking to other people you don’t know very well (or don’t know at all), Collins has some suggestions. When he moved to a new city, he signed up for a guitar lesson to meet other adults. If musical elegance is rarely your thing, you can sign up for a hiking organization or an e-book club.
During the pandemic, Collins began volunteering for a crisis helpline. You also need to call your friends to check if they rely on text conversations.
“It’s little things like that trump our concern about talking to people,” he said.
Discover advances in vaccination in California with our tracker.
Let’s start with some of the worst news noticed in nearly a year: In Los Angeles County, another 164 people died from COVID-19 in the week ending Wednesday.
We give you a lot of numbers in this newsletter, so you may have lost track of whether this number is the highest or the lowest. That’s the best thing: the highest weekly death toll the county has noticed in 10 months. By comparison, the worst week in L. A. CountyDuring the summer wave it left 122 dead.
It turns out that 164 can become the focus of winter attention. On Tuesday, the county’s weekly death count dropped to 159. But he is still there.
“Deaths are high and it’s concerning,” said Barbara Ferrer, Los Angeles County public health director.
It is not known why deaths have risen so much when the number of infections shown is low. In the summer, the weekly case rate peaked at 476 infections consisting of 100,000 county residents; In the existing wave, it peaked at 272 in line with 100,000 (the first week of December).
COVID-19 has been particularly fatal for seniors. In the last 3 months of 2022, the death rate for county citizens 80 and older is nearly five times higher than for other people 65 to 79 and older. Similarly, the mortality rate of more young older people five times higher than that of citizens aged 50 to 64.
Older adults have been more vulnerable to the coronavirus, but Ferrer speculated that’s even truer now because many have gone too long without a dose of the COVID-19 vaccine. Although 93% of county citizens over the age of 65 are fully vaccinated, only 38% of those eligible for Omicron booster have earned it. Ferrer called the figure “sobering” and said more reminders would save her from hospitalizations and deaths.
He also raised the possibility that some of the other people who contract the coronavirus may also have other viruses, such as RSV or flu, that make it difficult for them to recover.
The “triple outbreak” of the virus is worrying some Latino parents whose children attend Los Angeles’ unified schools. They called on the district to reinstate the mask mandate until the end of January (at least) and resume weekly coronavirus testing.
“We are concerned about a return to school without any transparent preventative fitness protocol implemented through LAUSD so that our youth do not breathe in the virus infection,” they wrote in a letter to the district.
The parents are members of an organization called Our Voice: Communities for Quality Education. Most of them are from multifamily or low-income families in East and South Los Angeles. but also the monetary stability of the extended family.
Superintendent LAUSD. Alberto Carvalho that students, teachers and other district staff wear masks to slow the spread of respiratory viruses. He also suggested that parents vaccinate their children against COVID-19. Dr. Smita Malhotra, the school district’s medical director, presented the same advice.
“Thanks to science, thanks to vaccines, thanks to therapy,” Malhotra said last week, “we are now in a position where COVID-19 . . . It is for. . . RSV and influenza. And so, as we enter this new season of acute respiratory illness, we treat it as we have treated all respiratory viruses.
Our Voices members don’t speak for all parents, and there are many who don’t need to see a return to the district’s strict coronavirus controls.
“The mask mandates and they were a total waste of our taxes,” said one Westside parent. “So much learning, mental/physical/emotional fitness has been lost. “
But the parents of Our Voices are not disappointed by anything. Countywide, the number of groups connected to schools and youth systems increased from 27 in early October to 64 the week before Thanksgiving to 226 just before winter break. Ferrer said the relative trend.
Speaking of schools and vaccines, a new report from the Centers for Disease Control and Prevention indicates that vaccination rates among kindergarteners nationwide dropped in the 2021-22 school year.
Typically, at least 94% of kindergarten students are vaccinated against measles, tetanus, and other diseases. That mark was lost in the 2020-21 school year, as the pandemic disrupted all kinds of physical care of the regime. The fact that the vaccination rate dropped to about 93% the following school year is likely a sign that vocal opposition to COVID-19 shots has undermined some parents’ confidence in vaccines in general, CDC officials said.
Back home: There are positive signs that the post-holiday increase that public fitness officials feared would not materialize. Official coronavirus infections in Los Angeles County, and across the state, have declined in recent weeks. And while this could be partly due to an unreliable number of cases, wastewater surveillance also suggests that virus levels are decreasing.
COVID-19 “has given the impression of being solid during the holidays,” said state epidemiologist Dr. Anna S. Simpson. Erica Pan, and the authorities hope that “we are out of danger. “
Los Angeles County reported 1,857 cases in the week ending Thursday, down 19 percent from last week. This equates to 129 cases in a week with a population of 100,000. (Anything above a hundred is high. )
The CDC says the county’s COVID-19 network is “average,” a designation shared with Orange, San Diego and Ventura counties. Riverside, San Bernardino and Santa Barbara counties have low levels of COVID-19 network. Only one county in California — Mariposa — is lately classified as “high. “
Officials said the country has recorded 59,938 COVID-related deaths since early December. The National Health Commission said 5,503 of those deaths were due to respiratory failure caused by COVID-19, with the rest being hospitalized patients who had COVID-19 as well as other conditions.
The wording of the announcement warned that there were possibly other COVID-19 patients who died at home.
Government officials said the “emergency peak” of the outbreak would likely have passed. The number of other people seeking treatment at fever clinics dropped from 2. 9 million on Dec. 23 to 477,000 last week, they said.
Outdoor health experts in China greeted the figures with skepticism. And the World Health Organization has renewed its call for the Chinese government to provide more information about its outbreak.
Dr. Albert Ko, an infectious disease physician at the Yale School of Public Health, said the official death toll in China is artificially low because the country counts COVID-19 deaths so narrowly. Patients meet this definition if they suffer respiratory failure and die in a hospital. — and hospitals are concentrated in big cities, he said.
Ko said he worries about other people going to rural spaces to celebrate the Lunar New Year.
“We are concerned about what will happen in China as this outbreak spreads to the countryside,” he said.
Today’s query comes from readers who need to know: When I wear an N95 mask, am I primarily attacked by other people’s germs or by them as well as mine?
The answer is that an N95 will do both, especially if used correctly, with a seal around the face.
“You’ll have it for yourself and you’ll have it for them,” Dr. Aaron E. said. Glatt, Chief of Infectious Diseases at Mount Sinai South Nassau in Oceanside, New York.
The same would be true for any mask, the lower the quality, the less coverage it will provide, in any direction.
You don’t assume that your mask is as effective at blocking other people’s germs as it is at blocking your own. For example, if you wear a normal surgical mask, you’ll do a smart job of catching your infectious droplets before they succeed in other people. But that might not give it the same coverage point of other people’s Omicron particles, said Dr. Luis Ostrosky, infectious disease leader at UTHealth Houston and Hermann Memorial Hospital.
We need to hear from you. Please email us your coronavirus inquiries and we will do our best to answer them. Wondering if your inquiry has already been answered? Check out our archives here.
This sunny area is a funeral home, and other masked people wait for the cremated remains of their loved ones.
The crowds at crematoria are just one indication that the death toll in China is worse than the government suggests.
Zuo-Feng Zhang, who chairs the epidemiology branch at UCLA’s Fielding School of Public Health, told Bloomberg that 59,938 sounds like a fairly accurate number of hospital deaths, but that “it could be the tip of the iceberg” when it comes to the total. Number of deaths from COVID-19 nationwide.
A report by Peking University estimated that 64% of China’s population had been infected with the coronavirus by mid-January. they have died since early December, Zhang said.
Followi
Karen Kaplan is scientific and medical editor at the Los Angeles Times. Before joining the clinical group, he worked in the Business section. He graduated from MIT and Columbia University.
Subscribe to access
Followi