Bonsoir. I’m Karen Kaplan, and it’s Tuesday, November 1. Here’s the latest news on what’s happening with the coronavirus in California and beyond.
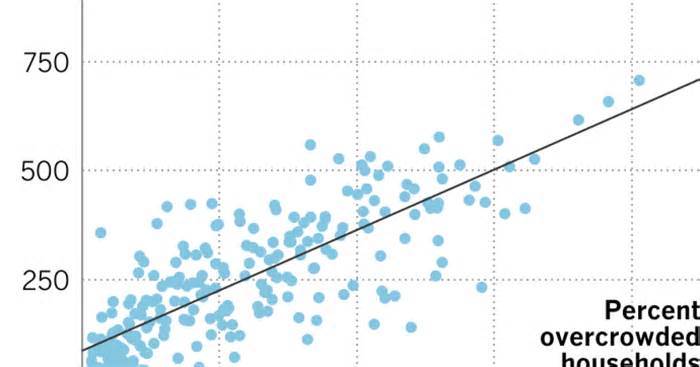
Take a close look at the chart below:
The X-axis on the back shows the consistent percentage of spaces in a specific neighborhood that are overcrowded, space more than one user according to the room (excluding bathrooms). The Y-axis along the left side measures the number of COVID-19 deaths consistent with 100,000 inhabitants.
Each blue dot on the graph represents a community in Los Angeles County. When you combine them that way, it’s pretty simple to see that the most populous communities also tend to have the highest COVID-19 death rates.
This point to the most sensible right corresponds to Pico-Union, a community just across the 110 freeway from downtown Los Angeles. Its 1. 33 square miles are home to about 40,000 residents, resulting in a population density higher than that of New York City. The Big Apple manages to pack millions of other people through the upward build. In Pico-Union, with no skyscrapers, they do this by cramming other people into houses and apartments.
The result is that 40% of families in Pico-Union are overcrowded. By comparison, the national average is 3%.
Having so many other people in such cramped neighborhoods has had fatal consequences for the other people who live there. The neighborhood’s COVID-19 death rate, 825 consistent with 100,000 citizens, is the time in the county. (The first position belongs to Lesser Armenia, where there were 1,172 deaths consisting of 100,000 inhabitants. )
Social distancing seems like everything can be done for free. But in crowded places, it’s a luxury that not everyone can afford.
Consider what happened at a Pico-Union residence: Leonardo Miranda, a 62-year-old structural worker, the coronavirus in December 2020. He lived in a shed in the assets but shared the bathroom, kitchen and dining room of the main house, where he passed the virus to a tenant sleeping in the laundry room. From there he jumped to Yelman Oviedo, 67, and his 18-year-old grandson, who shared some other room. Miranda and Oviedo died from COVID-19 15 days apart
The story is tragic at first glance, but there is one layer that makes it worse: The problem of overcrowding in Los Angeles County is the result of movements planned by civic leaders dating back more than a century, my colleagues Brittny Mejia, Liam Dillon, Gabrielle LaMarr LeMee and Sandhya Kambhampati Report.
Creating a sprawling oasis of single-family homes meant building apartments, skyscrapers or social housing complexes. Any of them would have improved the living conditions of the poorest inhabitants of the region. Instead, they had to sneak into the existing housing stock.
L. A. ‘s history begins after the Civil War, when it presented itself as an option for congested eastern cities. Those who wished to venture west would be rewarded with single-family homes with lush lawns, gardens, and fruit trees. be white, according to the rules of genuine heritage; the only option for other people of Mexican descent was to live in narrow shacks (where tuberculosis has spread as COVID-19 is lately).
Fast forward to the mid-1900s, when the Mexican neighborhoods of Chavez Ravine were razed to make way for a public housing allocation that was never built, displacing thousands of residents. Other assignments. One of those businesses in Boyle Heights drove about 10,000 people from their homes.
In the 1970s, the ‘slow growth’ movement put another impediment in front of those who would have benefited from high-density housing projects. “they have no choice yet to cram them into low-rise slums and change garages,” my colleagues write.
Since then, high housing costs have forced deficient citizens to double or triple, or worse, to the even worse fate of homelessness.
History makes it clear that the unjust decisions (to say the least) that were made decades ago still have consequences today. Manhattan Beach is about the same length as Pico-Union, but in this wealthy (and most commonly white) community, only 1% of families are crammed together, and the threat of dying from COVID-19 is 11 times lower.
Please take the time for the full story.
Case and in California at 4:55 p. m. Tuesday:
Track California’s coronavirus and vaccination efforts, adding the latest numbers and their breakdown, with our charts.
The other people who want COVID-19 vaccines the most are those most at risk of becoming seriously ill or dying if the coronavirus reaches them. The main ones are the elderly and other people with chronic diseases.
Unfortunately, the points they make can also complicate their ability to move on to a doctor, pharmacy, or vaccination clinic to get the vaccines they need.
Luckily for them, there are other people like Angela Tapia.
Tapia is a licensed nurse practitioner, one of seven or eight that the Los Angeles County Department of Public Health sends every day to vaccinate others at home. In total, the fitness branch has about 28 other people on its home vaccination team.
More than 7400 citizens of the county have been vaccinated through Tapia and his colleagues, adding more than 800 who have gained a reinforcement from Omicron.
Among them Maria Salazar, 88, bedridden with Parkinson’s disease. My colleague Emily Alpert Reyes was on her way home to Glassell Park when Tapia arrived to give her an encore.
“I’ll vaccinate you now, okay?” Tapia Salazar as her son, Louis, rubs her foot.
Tapia also gave Louis and his 90-year-old father injections while she was there.
“It’s a godsend,” Louis said, “especially for seniors who are confined to their homes. “
In fact, the only bad thing they told Alpert Reyes about the program is that it doesn’t reach more people.
“None of my patients had heard of the Los Angeles County Home Vaccination Program. None of the singles,” said Dr. Gene Dorio, an intern physician in Santa Clarita who specializes in geriatrics. I, they would never have known. My fear is how many more people don’t know about the program? »
County officials estimate that more than half a million people here may be confined to their homes. If so, the other 7,400 people who have been treated so far would make up 1. 5% of those who need vaccines.
Dr. Janina Lord Morrison, medical director of the cell vaccination team, said the program is promoted through doctors, Dório added, as well as through networks serving the elderly and on social media. But there is still a great lack of notoriety.
“The challenge is that other people just don’t know,” said Ernie Powell, president of Social Security Works California, an advocacy group.
The faster you can change, the better. Los Angeles County Public Health Director Barbara Ferrer said the number of county citizens who have won one of the new COVID-19 booster shots wants to “increase dramatically before the holiday season begins. “Otherwise, he said, the consequences will be felt more commonly. through “the elderly, other people with underlying physical conditions. It will make a difference in their lives. “
For his part, Morrison said his team will continue to deliver vaccines to county citizens, whether it’s bivalent boosters or the first COVID-19 vaccine. (Flu shots are also available. )People can request one from Tapia or one of his colleagues by calling (833) 540-0473 or filling out an online form.
“We will continue as long as other people ask us to,” Morrison said.
Learn about vaccination progress in California with our tracker.
It looks like the era of BA. 5, the Omicron subvariant so threatening that the FDA ordered new COVID-19 vaccines to counter it, may be coming to an end.
For the first time in months, BA. 5 accounted for less than a portion of coronavirus specimens circulating in the United States, according to estimates from the Centers for Disease Control and Prevention. At 49. 6%, however, it is even more unusual than any other strain of coronavirus.
But strains at points No. 2 and No. 3 are increasing. Over the past month, the presence of BQ. 1 increased from 1. 2% to 14% of U. S. specimens. Both are subvariants of BA. 5, and may have acquired sufficient adjustments to trump some of the immune coverage provided through new bivalent boosters or beyond BA. 5 infections.
A statement released last week through the World Health Organization’s Technical Advisory Group on the evolution of the SARS-CoV-2 virus said BQ. 1 and BQ. 1. 1 demonstrated “a significant expansion advantage” over other subvariants, and not just in the United States. His good fortune is likely due in part to “an immune evasion advantage,” the organization said. the chances of another COVID-19 outbreak.
It wouldn’t be the first time, Ferrer said. Emerging variants and subvariants of the virus have played a vital role in driving beyond outbreaks,” he said, adding that “we want to be prepared for the winter outbreak option. “
The WHO’s technical organization noted that lately there is no evidence that BQ. 1 or BQ. 1. 1 increase the risk of serious disease, or that existing COVID-19 vaccines are less effective in preventing serious illness.
The risk of pressure doesn’t exactly light the chimney under the Americans to get the new recalls from the market. According to the CDC’s most recent count, fewer than 23 million Americans have earned one. That’s only about 10% of those who are fully vaccinated (a number that’s stuck in 68. 4% of the U. S. population). UU. ).
The demand for injections increases with age. The CDC says 7. 3 percent of Americans age five and older have received bivalent booster. Among adults, this figure rises to 8. 6%. Even among the elderly, who are most likely to become seriously ill if they become inflamed, only 20. 1% rolled up their sleeves.
President Biden joined their ranks last week, updating his retreat in front of the cameras in front of members of his administration’s COVID-19 response team. Biden didn’t get his vaccine on his first outing because he fell with COVID-19 this summer and opted to wait a few months to spice up his immunity, like through the CDC.
He called on “all Americans to get vaccinated, as soon as they can” and said as many other people live within five miles of a position where they can receive the booster for free.
Speaking of vaccines, the Shanghai government has begun providing one that can be inhaled like a spray to be injected with a syringe. It is believed to be the first COVID-19 vaccine of its kind available to the general public.
In a Chinese state media video, a man inhaled the vaccine and held his breath for five seconds. The entire procedure lasted more than 20 seconds.
“It’s like drinking a cup of milk tea,” one of the recipients said in the video. “When I breathed it, it tasted a little sweet. “
Elsewhere in China, they left a Foxconn factory where iPhones are assembled because they feared the company wouldn’t protect them from COVID-19. According to social media, up to a portion of the factory’s 200,000 employees left the factory in the city of Zhengzhou.
A painter told reporters that the staff who fell had not received medical attention. A new mask mandate has been implemented, but other than that, the paints in the factory continue practically as before.
“There are still other people who are inflamed in the meeting lines and are still afraid to move to work,” said one employee who left the factory and was making plans to return to his hometown.
Lockdowns are back in Shanghai, where 1. 3 million citizens in a central community were ordered to retest for coronavirus and stay home until the effects returned. The order came Friday, a day when Shanghai, a city of 25 million other friends, reported 11 new infections, none of them symptomatic.
For some, it was reminiscent of the beginning of the two-month lockdown that swept the city earlier this year. Authorities first said the episode would only last a few days, but it ended up lasting so long that citizens faced food. shortage
Anti-COVID measures have been extended to Shanghai Disneyland, which temporarily closed Monday night, with visitors still inside, so workers and visitors can go through accelerated coronavirus testing, according to the city government. There are no main points about an outbreak imaginable at the theme park. have been released.
Reports on social media indicated that some of the attractions and other entertainment remained open to entertain visitors until it was their turn to try.
“Please go back and take a walk in the park,” a masked worker told visitors in a video posted on the Sina Weibo platform. “The gates of the park are temporarily closed and they can’t leave now. “
Today’s comes from readers who need to know: Have the main symptoms of COVID-19 changed?
You might be wondering if you’ve heard of a report from the Zoe Health Study, which uses an app to collect fitness data from legions of volunteers. In October, researchers leading the study, an organization from Harvard, Stanford and King’s College London, shared an update that revealed two attractive things about COVID-19.
First, most of the reported symptoms have actually changed. Compared to previous periods of the pandemic, other people who have health problems are now more likely to experience symptoms usually related to colds, flu, and allergies.
Sneezing, for example, has a very common symptom. This is consistent with the fact that Omicron infections tend to cause upper respiratory symptoms, whereas earlier strains were more likely to produce lower respiratory illnesses, such as pneumonia.
Symptoms such as muscle pain, chills and loss of taste or smell also disappeared from the most sensitive on the list.
The interesting thing about the moment is that the five maximum sensitive symptoms vary somewhat depending on the vaccination status. With that in mind, here are three separate lists of common new highs of COVID-19, starting with fully vaccinated people:
1. Sore throat 2. Runny nose3. Stuffy nose4. Persistent cough 5. Headache
For those who are not vaccinated, symptoms are:
1. Headache2. Sore throat 3. Runny nose 4. Fever 5. Persistent cough
And for those who won only one initial dose of vaccine, they are:
1. Headache2. Runny nose3. Sore throat4. Sneezing 5. Persistent coughing
These specific lists are found in the reports of other people suffering from COVID-19 in the UK, where new cases have emerged.
We need to hear from you. Please email us your coronavirus inquiries and we will do our best to answer them. Wondering if your inquiry has already been answered? Check out our archives here.
The device in the photo above is a pulse oximeter. These devices attach to a person’s finger and measure the amount of oxygen in their blood. They were most often discovered in hospitals, but the pandemic also brought them into homes.
A pulse oximeter works by sending two wavelengths of light to the skin and then measuring how much of that light is absorbed. These measurements make it possible to assess the amount of oxygen contained in the blood. But there’s a problem: the devices don’t take into account the gently absorbing properties of melanin, the pigment responsible for skin tone.
Therefore, pulse oximeter readings for other darker-skinned people might not be reliable. One study found that hospitalized black patients were nearly three times more likely than their white counterparts to have overall pulse oximeter readings, even when their actual oxygen levels were dangerously low.
Recent studies have documented negative consequences for patients of color, and now the Food and Drug Administration (FDA) is taking a closer look. The firm convened a panel of experts Tuesday to talk about what can be done to mitigate that racial disparity and make sure gadgets are for everyone.
“The fact that such a widely used device can make the slightest difference surprised me,” said Dr. Michael Sjoding, a pulmonologist at the University of Michigan who led the inpatient study. “I make a lot of medical decisions based on this device. “
Receive our free Coronavirus Today newsletter
Sign up to receive the latest news, stories, and what they mean to you, as well as answers to your questions.
You may get promotional content from the Los Angeles Times.
Follow
Karen Kaplan is scientific and medical editor at the Los Angeles Times. Before joining the clinical group, he worked in the Business section. He graduated from MIT and Columbia University.
Subscribe to access
Follow