Since the beginning of the pandemic, eating disorder providers have been involved with their patients.Those whose anorexia nervosa (AN), bulimia nervosa (BN) and binge eating (BED) were in remission began to worsen symptoms and new cases arose.This makes sense because restrictive nutrition is a way to control the uncontrollable, and during a pandemic, everything is uncontrollable.Feeding frenzy can also occur only because of the proximity of food, an emotional reaction to the pandemic, or even a food garage to prepare for self-storage.Until now, there was no knowledge to help what the doctors saw in the office.However, a new study through Termorshuizen et al published in the International Journal of Eating Disorders attempted to improve doctors’ perception of clinical and anecdote considerations and to directly examine how the pandemic affected others with eating disorders.
More than 1,000 participants in the United States (USA) And the Netherlands (NL) answered questions from qualitative and quantitative surveys.Among patients with self-formed NF, approximately two-thirds (62% of the US standard) were found to be in the united states.U.S., 69% of NL) reported an increase in restrictions and fears that they might be consistent with their eating plans.Increases in binge and binge craving episodes were reported through 30% of the US pattern.U.S. and 15% of the NL pattern they had,” BN and BED reported.When asked at Likert point (from “nothing involved” to “very involved”) about the effect of various Covid-19 stressors on their food disorders, the maximum non-unusual considerations were lack of structure, trigger environment, lack of support and lack of access to food in line with their eating plan.In the United States, 57% were also involved who could not exercise.
Dr. Jennifer Goetz, an assistant professor of psychiatry at Johns Hopkins School of Medicine who has a clinical appointment in the eating disorders program, said this exam supports what she sees in her clinical practice. She noted, “Many of my patients struggle with the disruption of their daily regimens and have a hard time adjusting to the lack of distribution [they] enjoy due to the various lockdown and painting / school restrictions. at home. “She, under pressure, the importance of the regimen in the remedy of eating disorders. This was echoed through Dr. Kristine Luce, psychologist and co-director of the Psychiatry Program in the Department of Psychiatry of Eating Disorders. Food in Adults from Stanford University School of Medicine, who said that one of the first interventions is “Establish a normal tendency to eat because the timing of meals has changed from hearing physical signals of hunger and satiety (feeling full ) to follow a rigorously enforced set of regulations to influence shape / weight.To do this, many patients will identify a tendency to dine around school, extracurricular activities and paintings and, as Dr. Goetz says, with virtual learning and running from home, this regimen is not the same.Even the smallest disturbance can make symptoms worse.
Although it was briefly discussed in the qualitative knowledge of the US, it was not the only one to be able to do so.As an explanation of why the worsening symptoms, experts singled out social media as a significant cause they see discussed clinically.Goetz believes that his teenage patient population spends more time, leading to a more direct comparison with others, which also happens with the shift from socialization and paintings to video platforms like Zoom, according to Dr.Ellen Fitzsimmons-Craft, assistant professor of psychiatry at the University of Washington School of Medicine and psychologist, who explains that being in a video makes the user look at himself more than the day or even in his free time, which can create anxiety by forcing the user to focus more on his appearance.
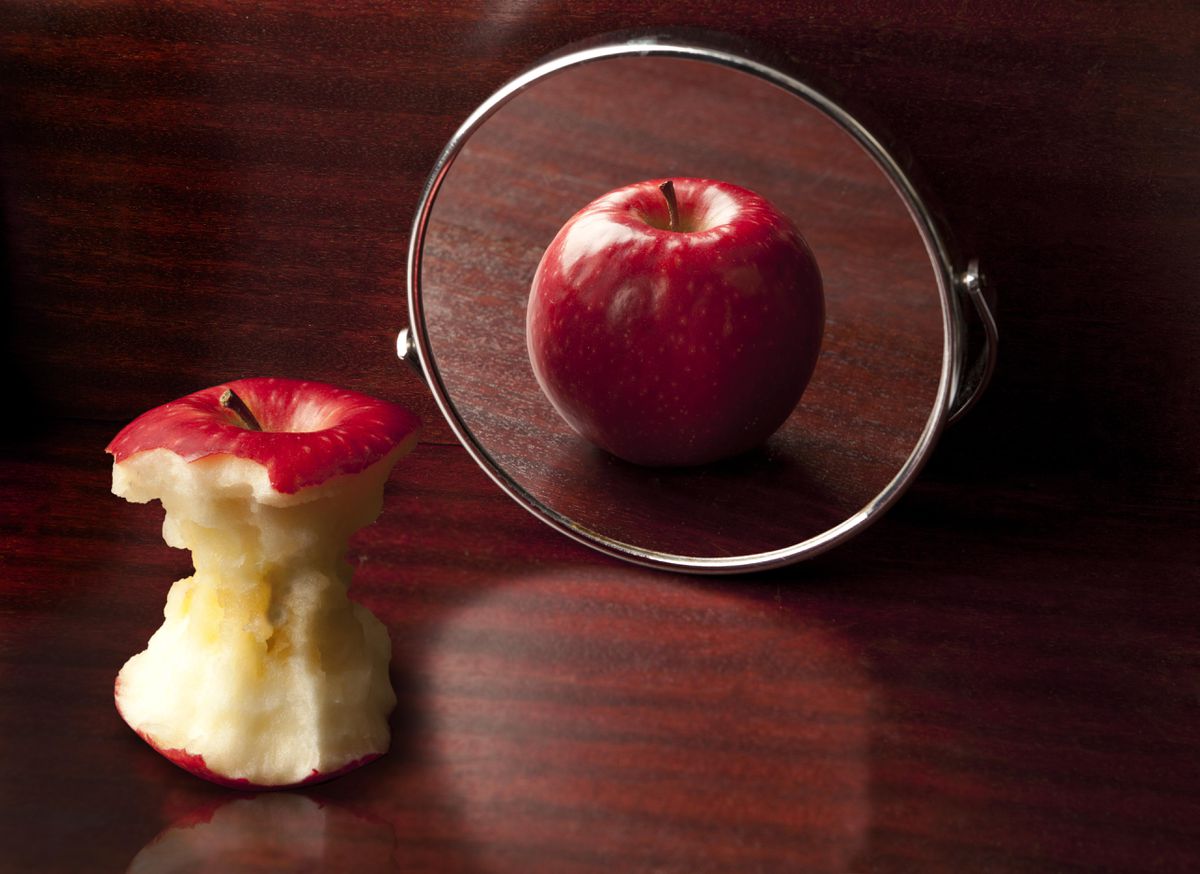
Dr. Goetz also comments that there have been many jokes about Covid-19 weight gain that have been particularly complicated for others with eating disorders and that have “caused the habit to get worse due to concerns about weight gain due to the pandemic itself.. Dr. Luce adds that she discovers the contradictory messages in our culture that the pandemic is difficult to reconcile.He explains that we have, for example, a “sedentary tax lifestyle that is continually noticeable in our culture”, while at the same time the gym is closed and our “accidental calorie burning”, such as going to the parking lot.from the desktop, is no longer available. Also, we have more people at home near their pantries and kitchens who are getting messages to eat “comforting food” when there’s not much to eat either.Other stimuli or methods of choice to deal with.In other words, balancing those messages around exercise, adaptation and food would be tricky for anyone, however, they are incredibly tr disgusting for those who are already at risk.
This comes with those with a solid record who feared a relapse.This organization reported an intake restriction (13% US, 13% NL) and compensatory behavior (5% US; 3% NL) in the study.Fitzsimmons-Craft notes that for others recovering from eating disorders it can be anything they want to be aware of and have the possibility to reappear, especially in times of maximum tension or transitions of life.She describes the pandemic as “as tense as possible.””and complete of many unforeseen primary adjustments in life (linkage, job loss, out-of-school children).Sometimes, during the tension, as Dr. Goetz points out, we resort to “safe and comforting” behaviors, which unfortunately can come with restrictions and bingees in which they have a history.
An attractive facet of this study is that it also showed positive effects of the pandemic on this population, with more than a third of respondents who said Covid-19 had led to positive adjustments in their lives.assisted to challenge your eating disorder behaviors and develop your motivation to recover.This is possibly due to the fact that, according to Dr. Goetz, some families now eat more meals together, which can decrease the triggering effect of the circle of family foods, help patients with more daily jobs and in the end normalize the diet.Moreover, as Dr. Fitzsimmons-Craft points out, without having as many activities and expectations as a result of the pandemic, there would probably be more time to devote to recovery-oriented goals and links.In other words, without so many stops to stop at and others to see, non-public care can nevertheless be a priority.
Furthermore, although this study attempted to discuss telehealth treatment disorders for this population, knowledge was limited. This was because the largest number of those who responded to the survey did not obtain any remedy at the start of the study (45% from the United States, 47% from the Netherlands), which is consistent with other studies. Importantly, those who had noticed a provider were able to transfer to telehealth with relative ease, but without further explanation as to why, many felt the quality of care was “a little” or “a lot” worse. However, anecdotally, some providers liked the transition. Dr. Shebani Sethi, founding director of the Metabolic Psychiatry Clinic at Stanford University School of Medicine and a qualified doctor of obesity medicine and psychiatry, notes that she enjoyed being able to visualize the surroundings of life, the pantry, and the kitchen of a patient. She believes this has made it less difficult for her to give helpful advice in ‘real time’, as’ educating the patient about eating [and] nutrition becomes less difficult when their food is right in front of either of us (visually for me ) rather just a talk about the office. Patients love it. Although it was out of necessity and telehealth has many flaws in this group, such as the inability to have physical exams or important symptoms (blood pressure, heart rate), other people may continue to receive mandatory care. a pandemic and that alone matters.
At the end of the day, we will have to stay in the brain that eating disorders are very common, progressive, recurrent and deadly diseases; in fact, eating disorders, as Dr. Goetz points out, have the highest mortality rate of all intellectual diseases., after deaths from opioid-related disorders.However, as she says, “in fact they don’t get as much attention or concentration as the maximum of the other diseases we treat.”It’s time for us to replace that, and it’s imperative that we don’t forget that these patients also suffer when we think about who has been affected by Covid-19.Because, as doctors predicted about eating disorders, and this test has shown that they actually have been.
Full policy and updates on the coronavirus
I’m an assistant professor of psychiatry at the University of Washington School of Medicine in St.Louis having been to the University of Pennsylvania (BA and M.S.)
I am an assistant professor of psychiatry at Washington University School of Medicine in St. Louis after studying at the University of Pennsylvania (BA and MA in anthropology), Yale School of Medicine (MD), and Stanford (adult psychiatry). ). I am primarily interested in the intellectual aptitude of the doctor, the intellectual aptitude in school, gender equality, medical education, suicide prevention and the overlap of popular media, stigma and psychiatry. I entered psychiatry for the love of patient stories and I think about storytelling, sharing and the patient’s experience. I teach medical and psychiatric interns, do research, share my views with colleagues at primary school medical centers and annual meetings, and publish my paintings in high-impact medical journals. I am also a company that believes in public education and promotion through the popular press as a doctor. As such, I am interviewed and talked to the media about all things intellectual aptitude, and my writing has appeared in, among others, The New York Times, Washington Post, TIME, Newsweek, Self, InStyle. and the HuffPost. I was also named one of Medscape’s Top 20 Social Media Influencers of 2019, primarily for my Twitter account (@drjessigold), where you can find me doing what I’m going to do here: protect patients and families, communicate on vital and applicable intellectual issues. Physical fitness issues destigmatize and normalize verbal exchange on intellectual fitness and communicate about media representations of intellectual illness as they arise.